16 May 2025, by Abdolghder Pakniyat. Peer reviewed by Shahriar Lahouti.

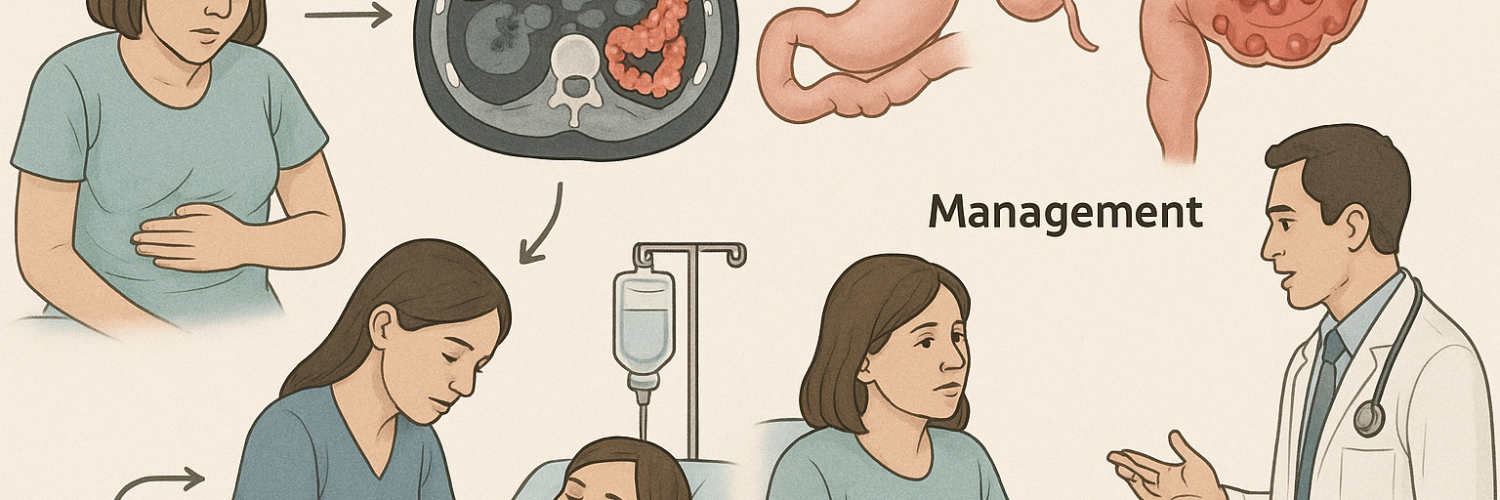
Diverticulitis is a condition where small pouches (diverticula) that can form in the lining of the digestive system, most commonly in the large intestine (colon), become inflamed or infected. While the presence of these pouches is known as diverticulosis and often causes no problems, diverticulitis occurs when these pouches become inflamed, potentially leading to symptoms such as abdominal pain, fever, and changes in bowel habits.
🔖 Step 1: Rapid Clinical Assessment
Quickly identify typical symptoms/signs:
-
Classic Presentation:
-
Sudden onset of constant LLQ pain (may radiate suprapubic or occasionally RLQ).
-
Low-grade fever, nausea ± vomiting.
-
Change in bowel habits (usually constipation; diarrhea less common but possible).
-
-
Physical Examination Pearls:
-
Localized LLQ tenderness (most common), mild guarding.
-
Mass (phlegmon/abscess) palpable ~20%.
-
Severe/diffuse tenderness, rigidity = suspect perforation/peritonitis immediately.
-
Caveats & Pitfalls:
-
Younger (<40 yrs) patients may present atypically; even RLQ pain is possible (mimics appendicitis).
-
Normal WBC/CRP doesn’t exclude the diagnosis.
🧪 Step 2: ED Diagnostic Workup
-
Labs Immediately:
-
CBC (WBC typically elevated but can be normal).
-
CRP (≥50 mg/L strongly supports inflammation/diverticulitis.
-
CMP (renal/electrolytes), urinalysis (rule out urinary tract disease/stones), pregnancy test (females).
-
-
Imaging Choice:
-
CT Abdomen/Pelvis (IV contrast preferred):
Why? It has high sensitivity (>95%) and specificity (~99%), clearly distinguishing uncomplicated from complicated disease and guiding management. -
Alternative imaging:
Ultrasound if CT unavailable (operator-dependent, less sensitive).
-
Avoid:
-
Plain abdominal X-ray (very limited role).
🩻 Step 3: Interpret Your CT Findings
-
Uncomplicated diverticulitis (Hinchey 0–Ia):
-
Bowel-wall thickening, inflammatory stranding, NO abscess, perforation, obstruction, fistula.
-
-
Complicated diverticulitis (Hinchey Ib–IV):
-
Abscess formation, perforation (micro or macro), obstruction, and fistula formation clearly seen.
-
🎯 Step 4: Decide Admission vs Discharge
Admission Criteria (if ANY apply → Admit):
-
CT shows complicated diverticulitis (abscess ≥4cm, perforation, obstruction, fistula).
-
Systemic signs (Sepsis/SIRS): fever ≥38°C, tachycardia ≥90, tachypnea ≥20, elevated WBC/CRP, markedly elevated.
-
Age ≥70 yrs
-
Immunocompromised (chronic steroids, chemotherapy, transplant, HIV).
-
Significant comorbidities:
-
Poorly-controlled diabetes, recent MI/CHF exacerbation, severe liver or renal disease.
-
-
Severe, uncontrolled pain despite analgesics in the ED.
-
Unable to tolerate oral intake (PO).
-
Poor home support or unreliable follow-up.
-
Failed outpatient management.
Who Admits?
-
Complicated diverticulitis: Surgery (colorectal/general).
-
High-risk uncomplicated patients (age, severe comorbidity, immunosuppression): Hospitalist/Internal medicine. Surgery consulted if not improving within 48–72 hours.
🏥 Step 5: Initial ED Treatment (while awaiting admission/disposition)
-
Pain Control:
-
IV acetaminophen ± opioids initially.
-
-
NPO initially → Clear fluids when disposition decided.
-
IV Fluids:
-
Normal saline or lactated Ringer’s bolus if dehydrated/hypotensive.
-
-
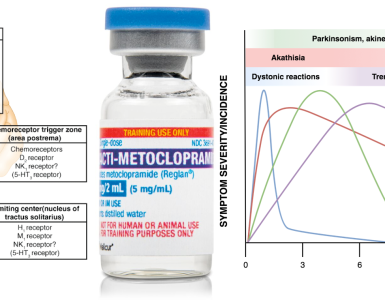
Antibiotics (if admitting or complicated):
-
IV Antibiotics recommended: Piperacillin-tazobactam or Ceftriaxone + Metronidazole.
-
-
Immediate Surgical Consult: for complicated diverticulitis cases.
🏠 Step 6: Clear Outpatient Management (Low-Risk Uncomplicated)
Discharge criteria (ALL required):
-
Uncomplicated diverticulitis confirmed by CT.
-
Age <70, immunocompetent, minimal comorbidities.
-
Adequate oral analgesia controls pain.
-
Tolerating clear liquids orally in ED.
-
Reliable outpatient follow-up within 48–72 hours.
Discharge instructions clearly include:
-
Clear liquid diet initially → advance slowly over 2–3 days.
-
Oral analgesics: acetaminophen ± short opioid prescription as needed.
-
NO routine antibiotics for uncomplicated, immunocompetent, low-risk patients.
-
Strict instructions for return (fever, worsening pain, inability to drink fluids, severe vomiting).
-
Arrange follow-up within 48–72 hours.
-
Colonoscopy planned 6–8 weeks after recovery (mandatory if first episode or complicated).
🏥 Step 7: Inpatient Management Essentials
Typical Admission Orders:
-
Admit to internal medicine (uncomplicated but high-risk) or surgery (complicated).
-
IV fluids and analgesics (initially NPO, then clear liquids as pain subsides).
-
IV antibiotics (Piperacillin-tazobactam or Ceftriaxone + Metronidazole).
-
Daily labs (CBC, CRP), abdominal exams.
-
Consult IR urgently for abscess ≥4cm drainage.
-
Consult surgery urgently for perforation, obstruction, or fistula.
-
Repeat CT imaging if no clinical improvement within 48–72 hours.
Criteria to transition to oral antibiotics and consider discharge from hospital:
-
Pain controlled orally, tolerating a regular diet.
-
Afebrile, normalizing vital signs.
-
Clear outpatient follow-up instructions and colonoscopy scheduled.
⚠️ Step 8: Common Pitfalls to Avoid in the ER
-
Overuse of antibiotics: Do not prescribe antibiotics to every diverticulitis patient. Reserve them for high-risk or complicated cases only.
-
Missing complicated diverticulitis: Any signs of peritonitis, severe pain, high inflammatory markers, advanced age → always consider complicated disease.
-
Delay in surgical consult: Early involvement prevents complications.
-
Poor discharge instructions: Explicitly explain red-flag symptoms and follow-up clearly to avoid bounce-backs.
📌 Quick, Practical Takeaways:
-
Clearly classify diverticulitis (uncomplicated vs complicated).
-
Admit complicated/high-risk patients promptly.
-
Select appropriate admitting service clearly: Surgery vs Medicine.
-
Follow clear criteria for safe outpatient management.
-
Communicate discharge instructions explicitly.
References :
- PMID: 33279517. Peery AF, Shaukat A, Strate LL. AGA Clinical Practice Update on Medical Management of Colonic Diverticulitis: Expert Review. Gastroenterology. 2021 Feb;160(3):906-911.e1. doi: 10.1053/j.gastro.2020.09.059. Epub 2020 Dec 3.
- PMID: 32384404. Hall J, et al; Prepared on behalf of the Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Left-Sided Colonic Diverticulitis. Dis Colon Rectum. 2020 Jun;63(6):728-747. doi: 10.1097/DCR.0000000000001679.
- PMID: 30625484. Nagata N, Ishii N, Manabe N, Tomizawa K, Urita Y, Funabiki T, Fujimori S, Kaise M. Guidelines for Colonic Diverticular Bleeding and Colonic Diverticulitis: Japan Gastroenterological Association. Digestion. 2019;99 Suppl 1:1-26. doi: 10.1159/000495282. Epub 2019 Jan 9.
- PMID: 35063008. Fugazzola P, et al. The WSES/SICG/ACOI/SICUT/AcEMC/SIFIPAC guidelines for diagnosis and treatment of acute left colonic diverticulitis in the elderly. World J Emerg Surg. 2022 Jan 21;17(1):5. doi: 10.1186/s13017-022-00408-0.
- Winters ME, Woolridge DP, Marcolini E, Lu M, Dubbs SB. “Avoiding Common Errors in the Emergency Department.”


Add comment