9 December 2022 by Shahriar Lahouti
CONTENTS
- General principles
- Shoulder joint
- Elbow joint
- Hip joints
- Knee dislocation
- Ankle dislocation
- Appendix
- Going further
General principles
- Terminology
- The proper terminology for dislocations describes the relationship of the distal (or displaced) segment relative to the proximal bone or the normal anatomic structure. The terms anterior and posterior are used for most major joints dislocations. For example, if the head of the humerus lies anterior to the glenoid fossa, the injury is an anterior shoulder dislocation.
- History
- Mechanism of injury: Provides a diagnostic clue to associated injury.
- Prior history of dislocations and how long the joint has been dislocated.
- Examination
- Visual inspection: see how the patient is holding the affected extremity, look for deformities, alterations of normal joint contour, and any overlying skin changes (lacerations, bruising, or swelling).
- Palpation: Assess the bones/joints and any surrounding musculature for tenderness, step-off, crepitus, warmth.
- Range of motion (ROM); both active and passive.
- Examination of the joint above and below.
- Neurovascular assessment
- For all dislocations, document neurovascular status of the extremity both before and after the reduction.
- Vascular exam: Significant vascular injury is assessed by↓ or absent distal pulses, ↑capillary refill time, pulse oxymetry distal to the injury and comparing the results with those of the uninjured extremity, Doppler ultrasound, and looking for development of an expanding hematoma.
- Neurological exam (see upper and lower extremity neuroexam)
- Assess for signs of compartment syndrome.
- Pain: Unrelenting, non-positional, progressive and disproportionate pain is the most common finding.
-
Aside from pain out of proportion, the remaining symptoms above are often late findings in compartment syndrome.
- Palpation of firm compartments is not a reliable clinical finding *.
- The use of the five P mnemonic (pallor, pain out of proportion, pulselessness, parasthesia, and paralysis) to assess compartment syndrome is misleading. These signs are more often signs of arterial ischemia than acute extremity compartment syndrome *.
- Peripheral pulse exams are not reliable because compartment pressures are rarely high enough to occlude arterial blood flow *.
- Imaging
- Get appropriate radiographic assessment both before and after reduction.
- Distinguishing a fracture-dislocation before attempts at reduction (this may require orthopedic consultation; a consideration before such attempts).
- Imaging modalities may include plain Xray, bedside ultrasound, CT of the dislocated joint.
- CT angiography (CTA) is done when there is concern for arterial injury.
- Get appropriate radiographic assessment both before and after reduction.
- Reduction
- Timing of reduction
- It is generally accepted that the sooner a dislocation is reduced, the better. This is especially true in the presence of neurovascular compromise or skin penetration, where immediate reduction attempt is warranted.
- Preparation of the patient
- Analgesia with or without sedation
- There’s no solid accepted guidelines for the use of pharmacologic adjuncts in the management of dislocations.
- By enlarge, it is recommended to use pre-medication for majority of reduction performed in ER.
- Choosing the agents, and the dosage should be made individually each patient and dislocation type.
- Closely monitor the medicated patient.
- Alternatives to procedural sedation and analgesia include
- Intraarticular injection of local anesthetics
- Hematoma blocks
- Peripheral nerve blocks
- Regional anesthesia
- Analgesia with or without sedation
- Reduction technique
- Generally, reduction attempts should involve gentle, gradual application of force.
- This is especially true, for the dislocations accompanied by neurologic injury which should be reduced by the most expeditious and least traumatic method.
- It is important to know multiple reduction techniques as none works for every patient or type of dislocation.
- Generally, reduction attempts should involve gentle, gradual application of force.
- Irreducible dislocation
- A certain percentage of all types of dislocations are not amenable to closed reduction.
- Generally, this is not necessarily due to improper technique, rather it can be the result of following conditions
- Interposition of soft tissue structures or fracture fragments
- Inadequate sedation and analgesia
- Generally, this is not necessarily due to improper technique, rather it can be the result of following conditions
- Avoid several (two to three) unsuccessful attempts, and call for orthopedic consultation.
- A certain percentage of all types of dislocations are not amenable to closed reduction.
- Timing of reduction
- Post-reduction care
- Monitoring the medicated patient.
- Neurovascular exam.
- Passive range of motion (ROM)
- Full passive ROM should be tested for certain joints (e.g. elbow, hand, and forefoot joints) to assess the stability of the reduction and to ensure a smoothly gliding joint that is free of intraarticular obstruction.
- Be cautious for the shoulder, since full passive ROM may cause repeated dislocation.
- Rather, confirmation of reduction in shoulder joint can be evaluated by asking to place the palm of the ipsilateral hand on the contralateral shoulder.
- Immobilization: Adequate immobilization of the injured joint for comfort and to prevent repeated dislocation.
- Follow-up care: depend on the injury and its severity.
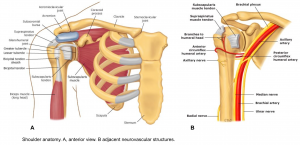
Shoulder joint
Anatomic consideration
- The glenohumeral joint has the greatest ROM of any joint in the body.
- These unique feature makes the shoulder joint, the most frequently encountered large joint dislocation.
- The anatomy of glenohumeral joint and major adjacent structures (e.g. axillary nerve is shown here).
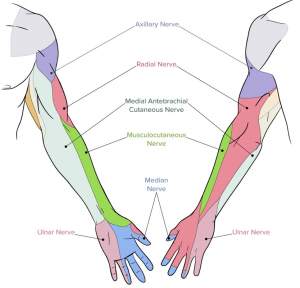
Upper extremity examination
- Inspection, palpation, ROM.
- Distal pulses
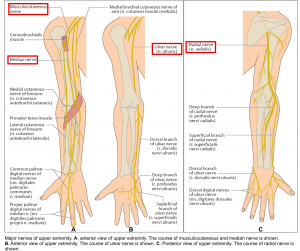
- Neurological exam: The course of major nerves of upper extremity is shown in figure below.
- Motor
- Musculocutaneous nerve (C5-C6). Motor innervation to biceps.
- Elbow flexion 💪.
- Reflex: Biceps reflex (C6)
- Axillary nerve (C5-C6). Motor supply to deltoid muscle (The course of axillary nerve is shown above)
- Arm abduction (from 15 to 90 degree). However it is difficult to assess in a patient with a dislocated shoulder, as it requires activation of the deltoid muscle.
- Radial nerve (C5-C8): Motor supply to extensor muscles (posterior compartment) of the arm, forearm and hand.
- Wrist and forearm extension
- “Thumbs up” 👍
- Reflex: Triceps (C8)
- Median nerve (C6-T1):
- Wrist flexion
- Make a fist ✊
- OK sign against resistance 👌(this will assess just the anterior interosseous branch of median nerve).
- Ulnar nerve (C7-T1): Motor supply to dorsal and palmar interossei, ( ulnar nerve injury causes impaired fingers abduction and adduction).
- Peace sign against resistance✌️
- Crossing index and middle fingers.
- Musculocutaneous nerve (C5-C6). Motor innervation to biceps.
- Sensory: It can be evaluated as following (see below figure).
- Axillary nerve: “Regimental badge” area over the deltoid muscle.
- Musculocutaneous nerve: Lateral forearm
- Radial nerve: Dorsal thumb, 1st web space
- Median nerve: Tip of the 2nd digit
- Ulnar nerve: Tip of the 5th digit
- Motor
Sensory innervation of upper extremity
The anatomic course of major upper extremity nerves
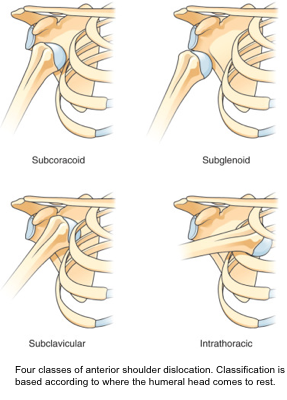
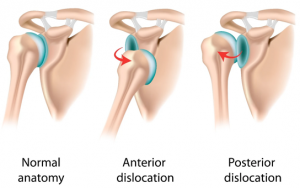
Epidemiology and classification of shoulder dislocation
- Shoulder dislocations account for 50% of all major joint dislocations.
- Classification (figure below)
- Anterior (~97%)
- Posterior (~<3%)
- Inferior (~<1%)
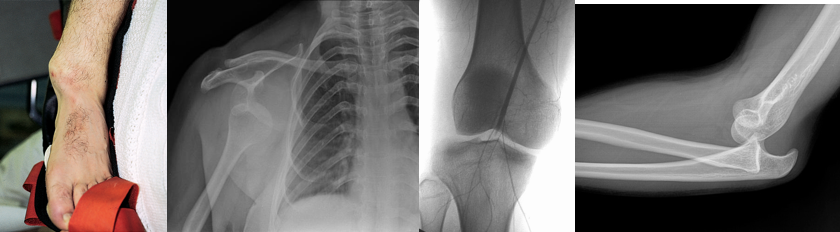
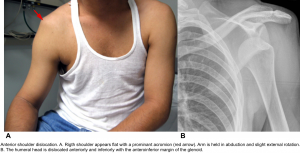
Anterior shoulder dislocation
- Most common type of shoulder dislocation (97%).
- The humeral head becomes situated in front of the glenoid fossa.
- Classification: Anterior dislocations are classified according to where the humeral head comes to rest:
- Subcoracoid dislocations (~75%). The humeral head is anterior to the glenoid fossa but inferior to the coracoid process.
- Subglenoid. Humeral head is anterior to the glenoid fossa but inferior to it as well.
- Subclavicular. Humeral head is anterior to the glenoid fossa but medial to the coracoid process and inferior to the clavicle.
- Intrathoracic. The humeral head is anterior to the glenoid fossa and also medial to the glenoid fossa, between the ribs.
Diagnostic considerations
- Mechanism of injury
- A fall onto palm with arm outstretched
- Direct blow to the posterior shoulder with anterior force
- Force/blow to abducted and externally rotated +/- extended arm (ie. Blocking basketball shot)
- Exam
- Loss of shoulder roundness (flattened appearance) with a prominent acromion.
- Arm is held in abduction and slight external rotation.
- Patient cannot adduct or internally rotate the shoulder.
- Any attempt at internal rotation is quite painful and resisted by the patient.
- Unable to place the palm from the injured extremity on the uninjured shoulder is consistent with an anterior shoulder dislocation.
- Neurovascular assessment
- The sensory component of the axillary nerve is assessed by testing for sensation over deltoid muscle (regimental badge” area).
- Imaging
- AP View: Humeral head dislocated anteriorly and rests under the coracoid process.
- Scapula Y View: humeral head displaced medially (to the right) of the scapula.
- Axillary view: Humeral head displaced anteriorly in front of the coracoid process.
- POCUS for shoulder dislocation here.
Associated injury
- Neurological deficit
- Axillary nerve injury (~5-13%) *: is the most common nerve injury resulting from anterior dislocations
- Rotator cuff injuries
- Humeral head fractures
- Axillary artery injury (rare)
Reduction
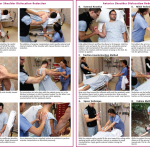
- Methods *
- There are over 20 different techniques for shoulder reduction, but no clear optimal method has been found *, *. See blow video for reduction by external rotation. For other methods refer to appendix 1.
- It is important to know multiple reduction techniques as none works for every patient or type of dislocation.
- There are over 20 different techniques for shoulder reduction, but no clear optimal method has been found *, *. See blow video for reduction by external rotation. For other methods refer to appendix 1.
- Post-reduction care
- After successful reduction, the patient’s shoulder should be immobilized (in internal rotation position) with either a commercially available shoulder immobilizer or a sling and swathe splint to limit external rotation and abduction.
- The duration of immobilization is controversial and multifactorial (e.g. age, first time vs. recurrent dislocation). By enlarge the average duration of immobilization is ~1 week.
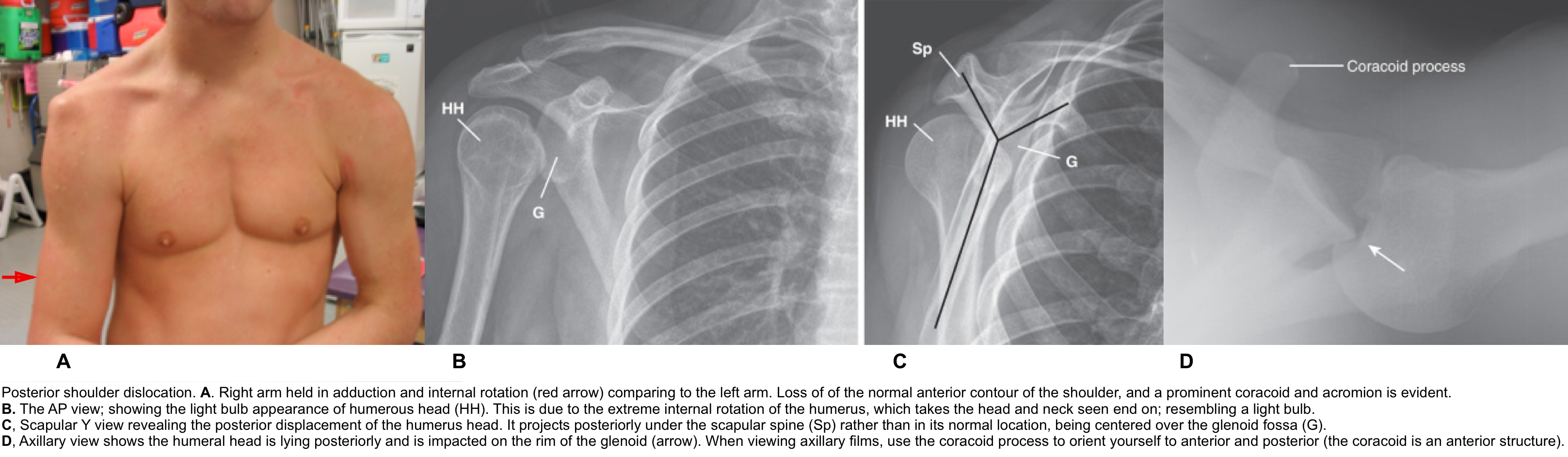
Posterior shoulder dislocation
Posterior shoulder dislocations are commonly missed because of subtle radiographic findings.
Diagnostic consideration
- Mechanism of injury
- Indirect injury consisting of a combination of internal rotation, adduction, and flexion force.
- Classic precipitating events include seizure, electrical shock, and falls *.
- Exam
- Loss of normal anterior shoulder roundness. The shoulder is flattened anteriorly and rounded posteriorly.
- Prominent coracoid and acromion.
- Arm is held in relatively fixed adduction and internal rotation.
- Abduction and external rotation are limited, and painful.
- Neurovascular exam
- Imaging
- The routine AP and lateral view, are potentially misleading and may result in misdiagnosing.
- The scapular Y and/or the axillary view reveal posterior dislocation of humerous head.
- POCUS for shoulder dislocation here.
Reduction
- Technique. See below clip
- Post-reduction care
- After successful reduction, the patient’s shoulder should be immobilized (in internal rotation position) with either a sling or a specialty brace.
- The duration of immobilization~1 week.
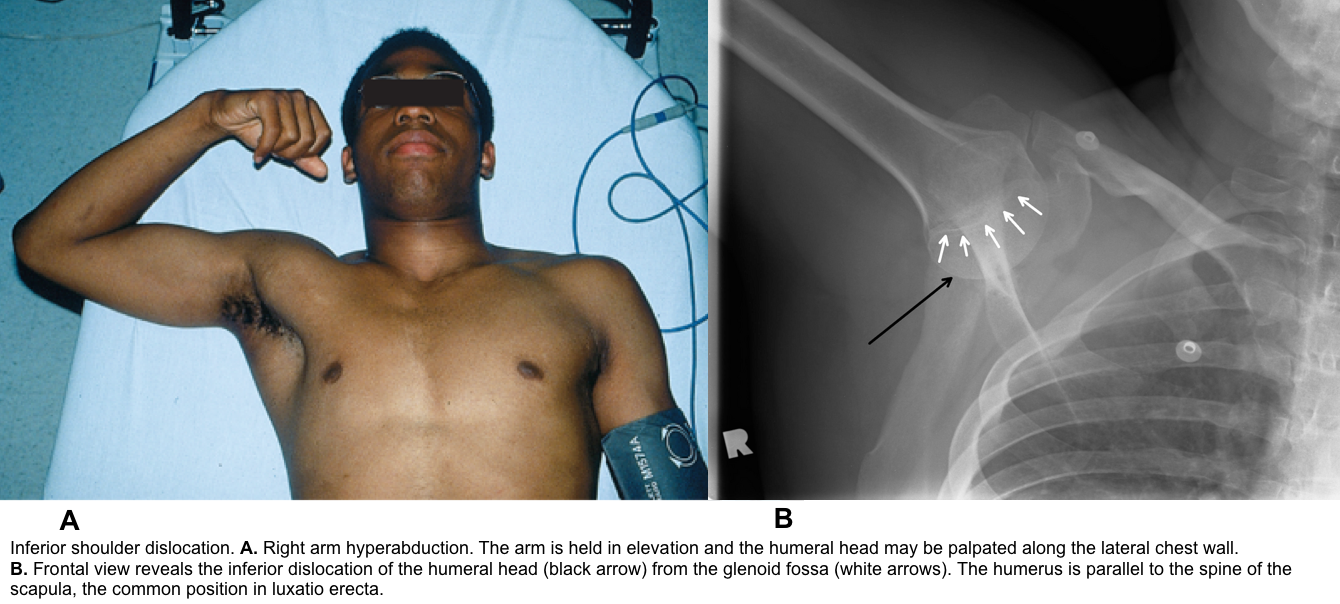
Inferior shoulder dislocation
Luxatio erecta is inferior glenohumeral dislocation (aka. Luxatio erecta). The humeral head is forced below the inferior aspect of the glenoid fossa due to a hyperabduction of the arm.
Diagnostic consideration
- Mechanism of injury: Two main mechanisms are described:
-
Hyperabduction force placed on the already abducted arm:
-
Proximal humerus is levered across the acromion, and the rotator cuff, along with the inferior and middle glenohumeral ligaments, are damaged.
-
-
Axial compression on a fully abducted arm:
-
This forces the head of the humerus through the inferior glenohumeral ligaments.
-
-
- Exam
- Loss of contour of the shoulder.
- The arm is held in marked abducted position with the elbow fixed and the forearm pronated.
- The humeral head can be palpated along the lateral chest wall.
- Neurovascular exam
- Imaging
- AP view shows inferior dislocation of humerous head.
- Radiologic differential diagnosis:
- An inferior dislocation can mimic a subglenoid anterior dislocation on, where the humeral head rests directly inferior to the glenoid in the AP and lateral projections. It is distinguished from the latter by the humeral shaft’s position parallel to the scapular spine.
Associated injury
- The inferior capsule is almost always torn.
- Fractures of the greater tuberosity, acromion, clavicle, coracoid process, and glenoid rim can happen *.
- Concomitant neurologic injury as high as 60% * (Axillary nerve and vascular injury).
Reduction
- Technique. Video below.
- Post-reduction care
- After successful reduction, the patient’s shoulder should be immobilized (in internal rotation position) with either a sling or a specialty brace.
- The duration of immobilization is ~1 week.
Elbow joint
Anatomic consideration
- The elbow joint is one of the most stable joints in the body. It is stabilized by a complex of tissue and structure including
- Articulation: These are radiohumeral, ulnohumeral and radioulnar articulation
- Ligaments: including medial and lateral collateral ligament complex
- Dislocation of an elbow requires a significant force.
- Because of this stability, any dislocation is expected to be accompanied by considerable soft tissue damage.
- Associated fractures of the radial head and coronoid process of the ulna are common.
Neurovascular exam
- Due to close proximity of the brachial artery and ulnar and median nerves to the elbow, there are potential risk of neurovascular injury.
- Median and ulnar nerve exam.
Epidemiology and classification
- Elbow dislocation is the second most common dislocation, comprising 20% of all joint dislocations.
- In children this is the most common type of dislocation *.
- Elbow dislocations are usually simply divided into posterior and anterior dislocations.
- An isolated dislocation without fracture is “simple.” If an elbow dislocation is associated with a fracture (fracture-dislocation), it is called “complex.”
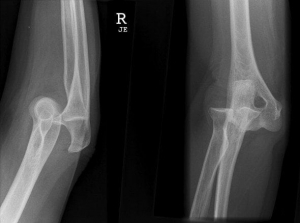
Posterior dislocation
Diagnostic consideration
- Mechanism of injury: fall on an outstretched hand with the elbow in extension.
- Exam
- Prominence of olecranon.
- Elbow is held in flexion.
- Imaging: The diagnosis is obvious with AP, lateral views. Consider oblique view or elbow CT scan for extra-articular fracture.
- Look for fractures of the distal end of the humerus, radial head, and coronoid process which are common in this injury.

Reduction
- Technique. See the video below.
- Post-reduction care
- Perform full ROM of elbow to make sure that the reduction is stable and there is no mechanical block to movement.
- An inability to move the elbow through a smooth ROM after reduction is often caused by an entrapped medial epicondyle fracture fragment, which requires operative intervention.
- Immobilize the elbow in at least 90 degrees of flexion with the forearm in slight pronation by using a long arm posterior splint.
- It is crucial that a patient has follow-up scheduled with an orthopedic surgeon within a week because early range of motion should be resumed within 5 to 7 days after the injury to prevent joint stiffness
- Perform full ROM of elbow to make sure that the reduction is stable and there is no mechanical block to movement.
Anterior elbow dislocation
Diagnostic consideration
- Mechanism of injury: Direct force to posterior forearm while elbow is in flexion
- Exam
- Olecranon is not prominent and is difficult to palpate.
- Elbow held in full extension, upper arm appears shortened with forearm held in supination and elongated
- Imaging
- Reduction
- Apply in-line traction and backward pressure on the proximal end of the forearm. An assistant provides countertraction by grasping the humerus with both hands *.

Radial Head Subluxation (Nursemaid’s Elbow)
- This is a common pediatric orthopedic issue. The pathologic lesion is generally a tear in the attachment of the annular ligament to the periosteum of the radial neck, with the detached portion becoming trapped between the head of the radius and the capitallum.
Diagnostic consideration
- Mechanism of injury
- The classic mechanism of injury is longitudinal traction on the arm with the wrist in pronation, as occurs when the child is lifted up by the wrist.
- Exam
- The arm is held slightly flexed and the wrist pronated at the side (nursemaid’s position)
- The child will refuse to use the arm. There is resistance or pain with supination.
- Palpation: There’s no/minimal tenderness in the radial head area.
- Imaging
- There’s no need to obtain X-ray for a child with an arm in the nursemaid’s position that is not tender (or minimally tender in the radial head area) on palpation and an appropriate history (classic nursemaid’s elbow).
- Indication for X-ray
- No typical history of injury
- Tenderness over radial head
- External signs of trauma (e.g. swelling, abrasions, ecchymoses).
- If the child has not regained use of the arm after a few attempts (2-3 attempts) within a reasonable period of time.
Reduction
- No need for procedural sedation
- Technique
- Supination method (video below).
- Pronation method: the forearm is not supinated. Instead, the forearm is rapidly hyperpronated and flexed. A review study concluded hyperpronation to be more successful and less painful than the supination method.
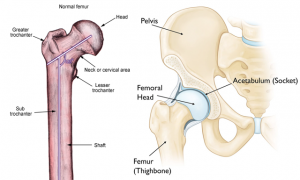
Hip joint
Anatomic consideration
- The hip is an inherently stable ball-and-socket joint.
- It requires a significant amount of force (at least 90 pounds) to be dislocated.
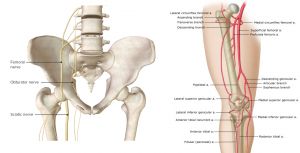
Neurovascular examination of lower extremity
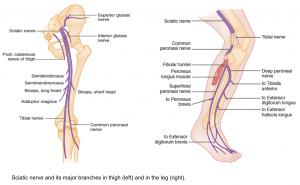
- The anatomic relationship of sciatic nerve, femoral nerve to hip joint and major arterial system of lower extremity is shown below.
- Sciatic nerve injury commonly (~10%) happens in posterior dislocation of the hip.
- Avascular necrosis of femoral head is another frequent complication of hip dislocation.
- The risk of neurovascular injury is high in major joints dislocation of lower extremity.
- Often times, a complete neurological exam is not required and is time consuming. Rather, focused neuro exam of the possible injured nerve bundle for each specific joint dislocation is more helpful. This task cannot be accomplished without basic neuroanatomic knowledge of lower extremity nerves. In the following figures, the sciatic nerve pathway through the thigh and lower leg is shown.
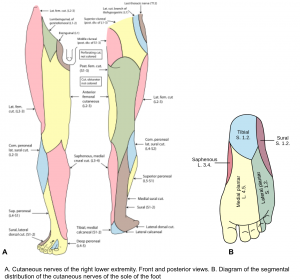
The major lower extremity nerves motor and sensory functions is reviewed here. The cutaneous innervation of lower extremity is shown below.
- Femoral nerve (L1-L4)
- Motor: Knee extension
- Sensory: Anteromedial thigh and anteromedial/posteromedial leg (via saphenous nerve, a sensory branch of femoral nerve). See figure. A below.
- Reflex: Patellar reflex (L4)
- Sciatic nerve (L4-S3)
- Motor: Knee flexion
- Sensory: It has no sensory branch
- Branches: It give rise to “common peroneal nerve” and “tibial nerve”👇.
- Common peroneal nerve: A branch of sciatic nerve. It wrap around the fibular head and give rise to
- Deep peroneal nerve (L4-S1)
- Motor: Ankle and great toe dorsiflexion
- Sensory: First toe web space (figure. A, below)
- Superficial peroneal nerve (L5-S1)
- Motor: Foot eversion
- Sensory: Dorsal foot (figure. A, below)
- Deep peroneal nerve (L4-S1)
- Tibial nerve (L5-S2)
- Motor: Ankle plantar flexion, flexion of the toes
- Reflex: Ankle reflex (S1)
- Branches:
- Sural nerve: A pure sensory branch of tibial nerve which arises in popliteal fossa. See the below figure for sensory innervation of foot and leg.
- Tibial nerve terminates in the foot by dividing into medial and lateral plantar nerves.
- Medial plantar branch of tibial nerve
- Motor: Flexion of the first 4th toes
- Sensory (figure. B, below)
- Lateral plantar branch of tibial nerve
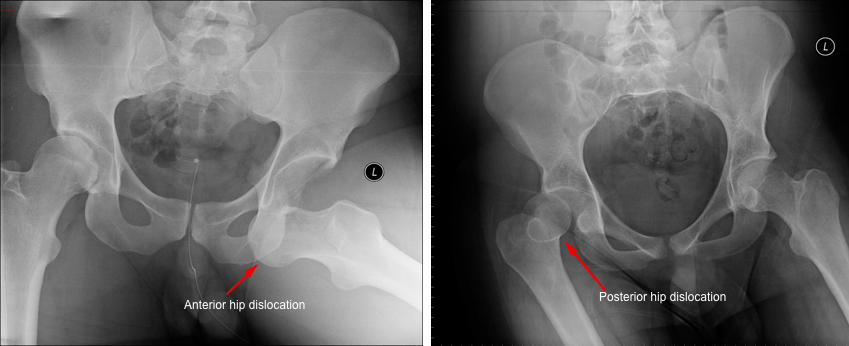
Hip dislocations
Epidemiology and classification
- Hip dislocations account for 2% to 5% of all joint dislocations.
- Classification
- Anterior dislocation (~90%). Femoral head is anterior to the acetabulum. Anterior dislocations are further divided into:
- Inferior (~90%)
- Superior (~10%)
- Posterior dislocation (~10%): Femoral head is posterior to the acetabulum
- Anterior dislocation (~90%). Femoral head is anterior to the acetabulum. Anterior dislocations are further divided into:
- Bilateral hip dislocations occur approximately 1% of the time.
Associated injuries and complications
- Fractures: Associated fractures (~88%) are common with hip dislocations.
- Sciatic nerve injury: Seen with ~12% of posterior hip dislocations.
- Avascular necrosis of the femoral head
- As the femoral head dislocates, it can injure the femoral neurovascular bundle. Diminishes blood supply to the femoral head leading to avascular necrosis.
- Delay to reduction is associated with higher rates of avascular necrosis; however, this can also occur with short reduction times.
- Nevertheless, it is still advisable to reduce hip dislocations as soon as feasible to decrease soft tissue distortion. Avascular necrosis can develop within 6 hours stressing the need for prompt identification and reduction
- Reduction < 6 hours: 4.8% avascular necrosis
- Reduction > 6 hours: 52.9% avascular necrosis
- Nevertheless, it is still advisable to reduce hip dislocations as soon as feasible to decrease soft tissue distortion. Avascular necrosis can develop within 6 hours stressing the need for prompt identification and reduction
Diagnostic consideration
- Mechanism of injury:
- Anterior dislocation
- Axial loading of hip in extension and abduction
- A significant posterior force on the joint forcing the femoral head anteriorly.
- Axial loading of hip in extension and abduction
- Posterior dislocation
- Axial loading of hip in flexion and adduction.
- Dashboard injury where the patient’s knee hits the dashboard/steering wheel in flexion and forces the femoral head posteriorly.
- Anterior dislocation
- Exam
- Anterior dislocation: Mildly flexed, abducted and externally rotated lower extremity.
- Posterior dislocation: Flexed, adducted and internally rotated lower extremity.
- 👉Altered mental status or ipsilateral deformities of the femur or knee may obscure the diagnosis.
- Anterior dislocation: Mildly flexed, abducted and externally rotated lower extremity.
- Imaging: a plain hip with AP pelvis.
- If suspicion for associated fracture, subsequent CT is recommended to fully characterize the injury.
Reduction
- Principles
- Urgent reduction (<6 hours) should be performed in most cases to reduce the risk of osteonecrosis.
- If there is an associated hip/femoral neck fracture, the patient may require closed reduction under anesthesia or an open reduction in the OR.
- Technique:
- Numerous reduction techniques are described in the literature. Each technique, which generally disengages the femoral head from the acetabulum and uses inline traction *, has different advantages for efficacy, mechanical advantage, patient safety, and provider safety. None have been shown to have superior efficacy.
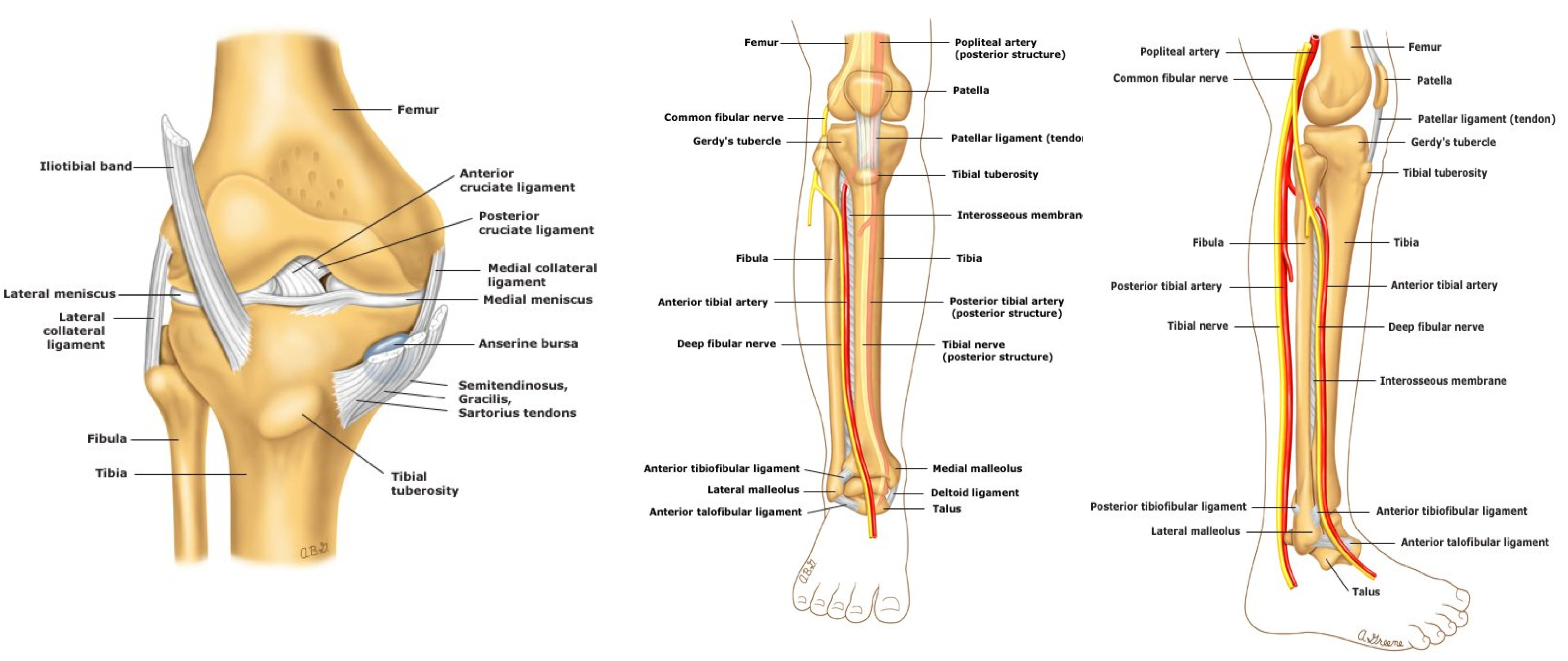
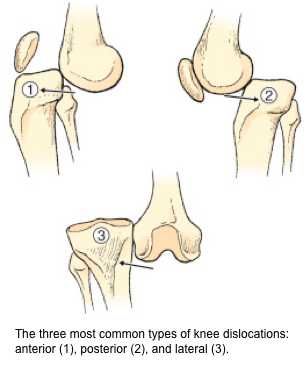
Knee dislocation
Anatomic consideration
- Knee dislocations are quite rare because of its strong ligamentous support. The major ligaments include the anterior and posterior cruciate and the collateral ligaments. Dislocation of knee joint always includes injury to one or more knee-stabilizing ligaments.
- High-velocity mechanisms are generally needed to cause dislocation of the knee.
Epidemiology and classification
- Knee dislocations account for less than 0.5% of all joint dislocations.
-
Approximately two-thirds of knee dislocations spontaneously reduce before initial presentation.
-
As a result, it is likely that the true incidence of knee dislocation is underestimated.
-
Spontaneous reduction may lead to missed or delayed diagnoses.
-
There needs to be a high index of suspicion to avoid these missed diagnoses
-
-
- Classification:
- The 3 more common types are shown below (anterior, posterior, and lateral).
- The less common types are medial and rotatory.
Associated injuries
- Popliteal artery: 40% of knee dislocations cause vascular injury.
- Posterior dislocations cause transection of popliteal artery.
- Anterior dislocations cause traction of popliteal artery.
- Common peroneal nerve: Travels around fibular neck
- Sensory to dorsal foot
- Motor dorsiflexion of ankle, extension of toes
- Tibial nerve *
- Sensory to posterolateral leg and lateral side of foot
- Plantar flexion of ankle and toes
- Fractures: Distal femur, proximal tibia, tibial plateau, and patellar fracture.
- Compartment syndrome
-
Intractable, severe pain out of proportion to injury and with passive stretch of the ankle and toes.
-
Diagnostic consideration
- Mechanism of injury
- Generally high-velocity forces are more likely to result in a dislocation.
- Have a high index of suspicion for dislocation is important as many dislocations have reduced spontaneously.
- Time of injury
- ⏳is important because vascular injuries are time-sensitive. Vascular injuries have a poor prognosis if repaired > 8 h after injury.
- Exam
- Pulse check
- Inspection
- Look for obvious deformity, swelling, and ecchymosis, and ability to move the knee.
- Gross deformity may be present or not (i.e. dislocation may have spontaneously reduced before evaluation in the ED and be manifested only as severe knee pain with hemarthrosis).
- A knee hemarthrosis, usually a large one with signs of posterior or calf hemorrhage, is a potential tip-off to a reduced dislocation.
- An effusion will often be absent since the capsule has been violated.
- ROM and assessment of knee stability: usually is not applicable due to pain and spasm.
- When to suspect an occult knee dislocation
- Three of the 4 knee ligament disruption or ligamentous laxity in multiple directions (a “loose knee”)
- A ‘buckling’ knee with a foot drop (common peroneal nerve palsy)
- If upon lifting up the patient’s leg by their heels the knee falls into hyper-extension compared to the contralateral knee
- High energy mechanism of injury or low energy mechanism in obese patients (with BMI>40)
- Imaging: X-rays, CT for fractures, CTA/MRA to evaluate vascular status.
- Indications for CTA/MRA
-
Patients demonstrating insufficient perfusion or any asymmetry in physical exam.
-
All patients with knee dislocation.
-
If ABI <0.9 in those without hard findings of ischemia.
-
- Indications for CTA/MRA

Reduction
- Technique
- The basic initial approach for all types of knee dislocation is to apply traction to the extremity. This alone is often all that is required for reduction because of severe disruption of the ligamentous support of the knee.
- For anterior dislocations, lift the distal end of the femur to effect reduction.
- For posterior dislocations, lift the proximal end of the tibia to complete the reduction.
- For medial, lateral, and rotatory dislocations, a similar approach is acceptable, with pressure exerted in the medial or lateral direction as needed.
- The basic initial approach for all types of knee dislocation is to apply traction to the extremity. This alone is often all that is required for reduction because of severe disruption of the ligamentous support of the knee.
- Post-reduction care
- Immobilize in long leg posterior splint at 15 degree flexion.
-
Prevent tension on popliteal artery
-
Reassess and document neurovascular status
-
Reassess pulses
-
Measure ABI
-
-
Distal pulses diminished or absent
-
Bruit or palpable thrill
-
Active bleeding
-
Expanding or pulsatile hematoma
-
Ischemic limb
-
Cold, cyanotic extremity
-
Loss of sensorimotor function
-
Ankle joint dislocation
Anatomic consideration
- The bony anatomy of the ankle consists of the articulation of the distal tibia and fibula with the talus.
- The ligamentous support of the ankle is quite strong, and pure dislocations are uncommon. Usually, there are associated fractures of the ankle joint.
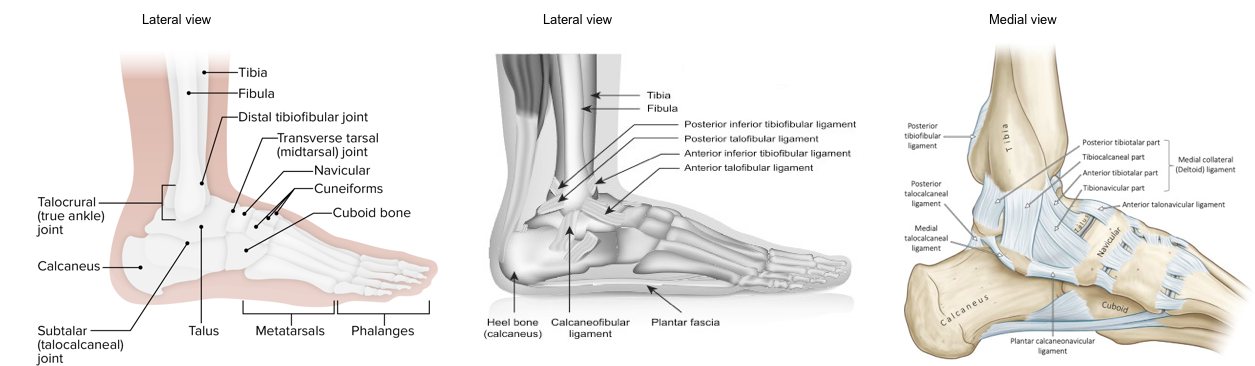
Epidemiology and Classification
-
Almost 30% of all ankle fractures have an associated tibiotalar dislocation *.
-
Pure ankle dislocations occur in 0.5% of all dislocations
- Ankle dislocations are described based on the position of the talus compared with the distal tibia.
- Posterior and lateral dislocations are the most common (see below).
- Other less common dislocations: medial, anterior, superior dislocations.
Diagnostic consideration
- Mechanism of injury
- It requires a tremendous amount of force to cause an ankle dislocation (motor vehicle accidents, falls, other high speed collisions).
- Axial-loaded force that eventually disrupts the joint capsule and ligaments and allows the talus to displace anteriorly or posteriorly.
- Exam
-
Gross deformity of the ankle.
-
Assess for signs of neurovascular compromise:
-
These include weak or absent dorsalis pedis and tibialis posterior pulses, as well as poor capillary refill.
-
Focused neurologic exam: Check for any movement of the great toe, plantar and dorsiflexion and gross sensation to the sole and dorsum of foot.
-
-
Tenting of the skin raises concern for necrosis and development of an open fracture.
- Assess for tenderness along the entire length of the tibia and fibula (esp. proximally near the knee) and a positive squeeze test. These findings may indicate a “Maisonneuve Fracture” (an important injury pattern involving the syndesmosis).
-
- Imaging:

Reduction
- Dislocations require rapid reduction *.
- Technique
- Posterior dislocations
- Grasp the foot with both hands; place one hand on the heel and the other on the forefoot.
- Apply traction on the slightly plantar-flexed foot.
- Have a second assistant apply downward pressure on the distal end of the tibia and move the heel anteriorly to affect reduction
- Anterior dislocations
- Apply traction on the slightly dorsiflex foot to free the talus.
- The second assistant applies upward pressure on the distal end of the tibia while the operator applies traction and pushes the foot in a posterior direction.
- Lateral dislocation
- Apply traction on the slightly plantar-flexed foot.
- Push the foot medially to affect reduction
- Posterior dislocations
- Post-reduction care
-
Reassess neurovascular status.
-
A posterior ankle splint (short leg splint) should be applied after reduction. The leg should be elevated immediately after reduction.
-
The patient should be non-weight-bearing.
-
Appendix
1.Anterior shoulder dislocation reduction techniques







Add comment