December 15, 2021 via Shahriar Lahouti
CONTENTS
- Potassium homeostasis
- Pathophysiology
- Clinical manifestation
- Diagnosis
- Causes of hypokalemia
- Investigation
- Treatment
- Potassium replacement
- Other therapeutic measures
- Disposition
- Further going
- Reference
Potassium homeostasis
Potassium is the main intracellular cation and almost all cells have the pump called sodium/potassium ATPase , that pumps sodium Na out of the cell and K into the cell leading to a K gradient across the cell membrane (Kin >K out), which is partially responsible for maintaining the potential difference across cell membranes. Many cell functions rely on this critically important potential difference such as neurons, cardiac myocytes, and muscle tissue.
Internal distribution of potassium
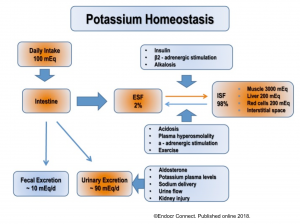
Only two percent of K exists in the extracellular fluid (ECF) at a concentration of only 4mEq/L, whereas 98% of exchangeable K is in the intracellular compartment. The regulation of K distribution between the intracellular and extracellular space is referred to as internal K balance.
- Under normal conditions, insulin and catecholamines play the most important role in this regulation (figure below) 1.
Patients with hypokalemia often have a large total-body potassium deficit. In a typical adult, a deficit of whole-body potassium of 100 mEq is required to decrease serum K by 0.3 mEq/L.
- K of 3 mEq/L may correlate with a potassium deficit of 100-200 mEq.
- K of 2 mEq/L may correlate with a potassium deficit of 400-600 mEq.
Estimation of the potassium deficit in clinical context depends on two factors
- The serum potassium level.
- The presence of any factors which may cause transcellular shift. For example, diabetic ketoacidosis causes potassium to shift out of the cells. Therefore, the potassium deficit may be even larger than would be estimated based on the above formula.
Since the vast majority of potassium in the body is located intracellularly, most of the total body potassium deficit represents deficient intracellular potassium. Therefore potassium replacement should be done slowly 🐌:
- Time⌛️ is required for potassium to enter the cells.
- Rapid administration may cause serum levels to be elevated (even though there is a total-body potassium deficit!). Serum hyperkalemia is dangerous ☠️.
Bedside clinical implications:
- IV K replacement should be done slowly.
- Even in severely hypokalemic patients, aggressive IV potassium administration can be dangerous; carrying the risk of severe hyperkalemia especially in following conditions
- Impaired renal function
- Presence of underlying redistribution mechanism of hypokalemia such as excess catecholamine, insulin, acidosis and thyrotoxic periodic paralysis.
- Rebound hyperkalemia can happen following reversal of underlying cause of hypokalemia. This can be prevented by slow replacement of K (if indicated).
Kidney potassium handling
External potassium balance is determined by the rate of potassium intake (normally 100mEq/day) and rate of urinary (normally 90mEq/day) and fecal excretion (normally 10mEq/day) (see figure above).
The kidney is primarily responsible for maintaining total body K balance. However, renal K excretion is adjusted over several hours; therefore, changes in extracellular K concentrations are initially buffered by movement of K into or out of skeletal muscle.
Potassium controls its own ECF concentrations through a feedback regulation of aldosterone release. An increase in K levels leads to a release of aldosterone through the renin-angiotensin-aldosterone mechanism or through the direct release of aldosterone from the adrenal cortex cells, which in turn increases urinary K excretion.
- More specifically, an increase in extracellular potassium concentrations stimulates aldosterone secretion (via angiotensin II), which in turn increases urinary K excretion.
In the steady state, K excretion matches intake and approximately 90% is excreted by the kidneys and 10% in the stool is fairly constant. By contrast, rate of K secretion by the distal nephron varies and is regulated according to the physiological needs.
- Mineralocorticoid activity: Aldosterone is the major mineralocorticoid and mediates the renal excretion of K and Na reabsorption by binding to the mineralocorticoid receptors in the distal tubules and collecting ducts of the nephron 2.
Potassium balance is closely related to magnesium balance, where hypomagnesemia is a common cause of hypokalemia, and should be considered when hypokalemia is identified. Hypomagnesemia results in an increased Na-K ATPase activity within the kidneys, and in the setting of hypomagnesemia, K is renally excreted regardless of whole-body K levels.
Pathophysiology
Decreased potassium levels destabilize the cardiac cycle through a number of mechanisms, resulting in slight depolarization of the resting potential and a resultant myocardial hyperexcitability with the potential to develop re-entrant arrhythmias.
- Although hypokalemia alone is likely not the primary cause of dysrhythmias. Rather, hypokalemia potentiates the arrhythmogenic effect of other conditions, such as long QT syndrome, ischemia, myocardial scarring, or other electrolyte abnormalities 3.
- Hypokalemia with concurrent hypomagnesemia can elongate the QT interval, especially in patients with pre-existing acquired long QT, and can predispose the patient to ventricular dysrhythmias, specifically torsades de pointes.
- A QT interval >500 ms increases the risk of torsades de pointes by 2 to 3 times 4.
Hypokalemia can cause rhabdomyolysis secondary to muscular ischemia mediated through a poor vasodilatory response 5 .
Hypokalemia affects a number of other electrolyte abnormalities. It can cause hypochloremia, hyperammonemia, and alkalosis by bicarbonate retention and may impair the renal concentration of pre-urine, resulting in polyuria.
Clinical manifestation
The severity of hypokalemia’s clinical manifestations tends to be proportional to the degree and duration of serum potassium reduction. Symptoms generally do not become present until serum potassium is below 3.0 mEq/L, unless it falls rapidly or the patient has a potentiating factor, such as the use of digitalis, in which patients have a predisposition to arrhythmias.
Mild hypokalemia (serum K 3-3.5 mEq/L) is frequently asymptomatic.
Moderate hypokalemia (serum K 2.5-3 mEq/L) can cause mild symptoms such as nausea, vomiting, abdominal distension, ileus 6 .
Severe hypokalemia (serum K < 2.5 mEq/L) can cause severe symptoms such as:
- Skeletal muscle cramps, fasciculation and tetany
- Paresthesia, numbness
- Hyporeflexia and weakness, typically ascending paralysis involving the diaphragm (the cranial nerves are usually spared)
- Tachydysrhythmias including “Torsade de point”
- Heart failure
- Rhabdomyolysis, myoglobinuria
Other manifestation of hypokalemia
- Glucose intolerance: Hypokalemia reduces insulin secretion, which may play an important role in thiazide-associated diabetes.
- Impaired renal concentrating ability causing nephrogenic diabetes insipidus.
- Worsening hepatic encephalopathy in patients with advanced cirrhosis.
- Worsening digoxin toxicity in those who take digoxin.
Diagnosis
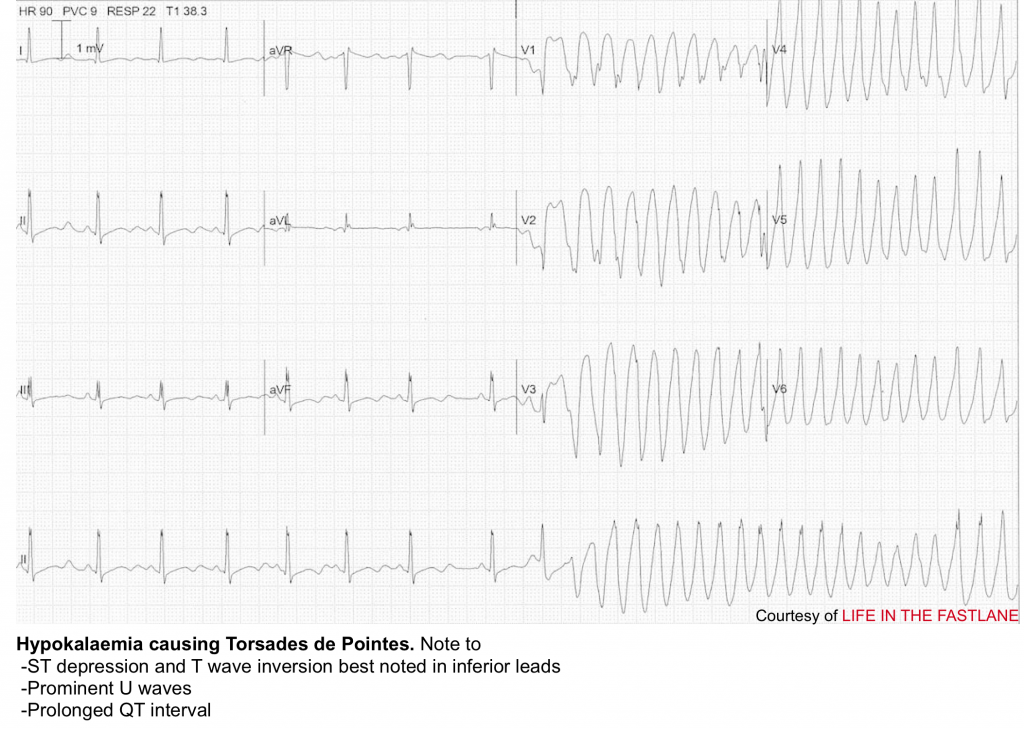
Diagnosis of hypokalemia is made when serum K of < 3.5 mEq/L. ECG changes generally do not manifest until there is a moderate degree of hypokalaemia (2.5-2.9 mEq/L).
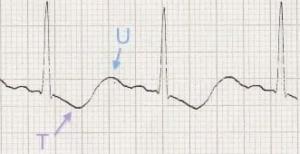
An ECG should be obtained from hypokalemic patients in the ED and may reveals
- T-wave abnormalities 7
-
- May flatten or invert. The earliest ECG manifestation of hypokalaemia is a decrease in T wave amplitude.
- Inverted T-waves followed by prominent U-wave may create a biphasic “down-up” morphology.
- U-wave prominence: may fuse with the T-wave to produce a prolonged QT interval.
- ST segments may appear depressed.
- QT prolongation, which may predict risk of arrhythmia.
- Arrhythmias
- Torsade de pointes may be the most classic.
- Other possibilities include atrial fibrillation, ventricular tachycardia, and ventricular fibrillation.
Red flags 🚩
The potential threat of hypokalemia relates to cardiac tachydysrhythmias. Risk factor associated with cardiac complication of hypokalemia include
- Severe hypokalemia ( < 2.5 mEq/L)
- Clinical context where potassium is likely to fall further (e.g. DKA or refeeding syndrome)
- Cirrhosis (hypokalemia can increase ammonia generation and promote the development of hepatic encephalopathy).
- ECG changes due to hypokalemia (e.g. QT prolongation, especially if QTc >500 msec ).
- Increased risk of arrhythmia ⚠️
By enlarge hyperkalemia is more dangerous than hypokalemia and in the absence of above risk factors, hypokalemia is well-tolerated.
Causes of hypokalemia
- Decreased oral intake: alcoholism, anorexia nervosa 1
- Potassium shift into the cells
- Beta-adrenergic agonist: albuterol, terbutaline, epinephrine; including endogenous epinephrine surges from stress
- Increased availability of insulin (e.g. during DKA resuscitation)
- Alkalosis
- Hypokalemic periodic paralysis (congenital type or acquired associated with hyperthyroidism)
- Hypothermia
- Chloroquine intoxication
- Marked increase in blood cell production
- GI loss: vomiting, diarrhea, large volume nasogastric suction, laxatives
- Renal loss
- Diuretics (carbonic anhydrase inhibitors, loop diuretics and thiazide-like diuretics) 10
- Hypomagnesemia
- Salt-wasting nephropathies, including Bartter’s or Gitelman’s syndrome
- Plyuria e.g post-obstructive diuresis, osmotic diuresis
- Mineralocorticoid excess
- Cushing syndrome
- Primary hyperaldosteronism
- Exogenous steroid
- Renal tubular acidosis type I or II
- Ampicillin, penicillin, aminoglycosides, amphotericin, foscarnet, cisplatin
- Dialysis
- Plasmaphresis
Investigation
- Review the medication list
- Review recent history e.g. diarrhea, polyuria, vomiting or gastric suction.
- Check a full electrolyte panel, the most important one is magnesium.
- BUN, creatinine
- Blood gas analysis: hypokalemia may be found with a metabolic alkalosis.
- Total serum creatine kinase in patients presenting with myalgias to screen for rhabdomyolysis induced by hypokalemia.
- Advanced diagnostic testing: Begin by checking urine potassium, creatinine, sodium, and chloride.
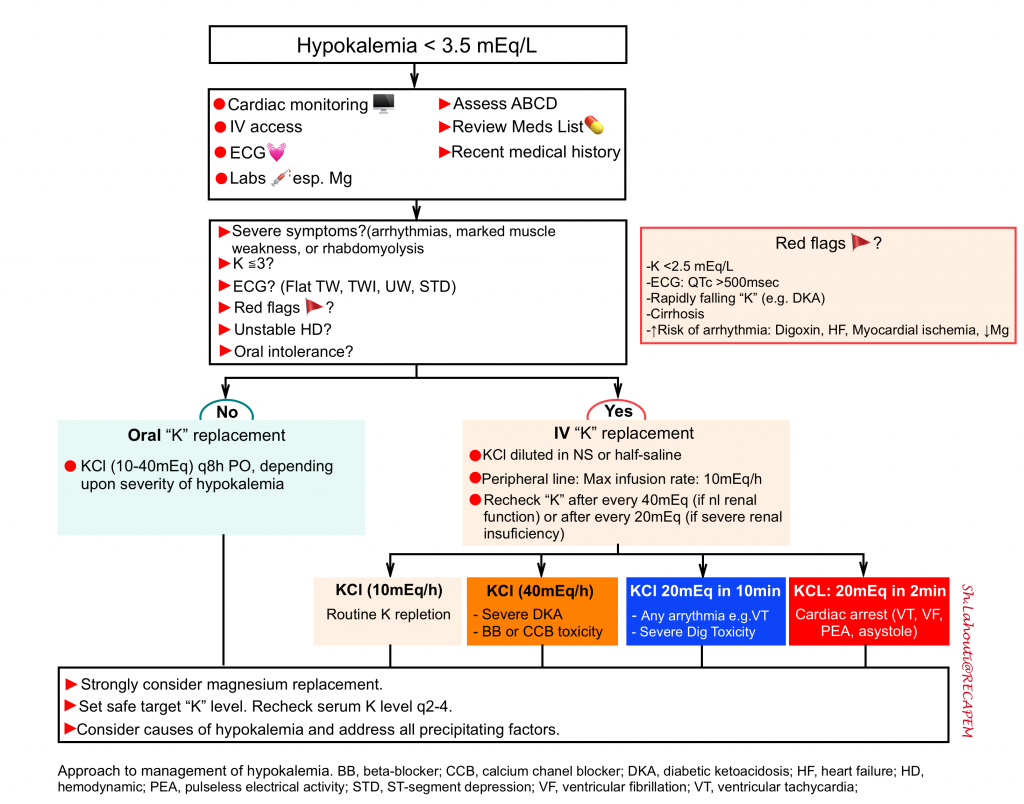
Treatment
The goals of therapy in hypokalemia are to prevent or treat life-threatening complications (arrhythmias, paralysis, rhabdomyolysis, and diaphragmatic weakness), to replace the potassium deficit, and to diagnose and correct the underlying cause.
The urgency of therapy depends upon the severity of hypokalemia, associated and/or comorbid conditions, and the rate of decline in serum potassium concentration.
The risk of arrhythmia from hypokalemia is highest in older patients, patients with organic heart disease, and patient on digoxin or antiarrhythmic drugs 17.
Treatment involves replacement of potassium. Magnesium depletion is very common in patients with hypokalemia and failure to treat the magnesium deficiency will make it difficult or impossible to fix the hypokalemia. General approach to management of hypokalemia is illustrated in following figure.
Potassium replacement
Target potassium level
- Targeting a potassium level >3.5 mEq/L for most patients including cardiac patients 16.
- Target a potassium level of >3 mEq/L for most patients with severe renal failure (in the absence of digoxin, myocardial ischemia or heart failure).
- For patients with DKA, target a potassium level >5mM/L.
- Patients being resuscitated from DKA will generally tend to drop their “K” levels over time.
- In the absence of renal dysfunction, it’s often useful to target a high-normal “K” level.
Route
- Oral replacement is safe, cheaper and easier.
- Indications: oral replacement can be considered in patients who meet all following conditions:
- Absence of red flags (above)
- Hemodynamically stable
- Mild hypokalemia (serum K >3 mEq/L)
- Able to tolerate oral intake
- Depending upon the severity of the hypokalemia treatment is usually started with 10 to 20 mEq of potassium given two to four times per day (20 to 80 mEq/day).
- For mild to moderate hypokalemia; KCl 10-40 mEq orally q8h to q12h can be administered (serum “K” level can transiently rise by as much as 1 to 1.5 mEq/L after an oral dose of 40 to 60 mEq).
- Indications: oral replacement can be considered in patients who meet all following conditions:
- Intravenous replacement (if indicated) should be performed under cardiac monitoring.
- Formulation: generally potassium chloride is used more frequently.
- Vehicle: potassium should be diluted in normal saline or half-saline. 👉Avoid administering K in glucose solutions (to reduce insulin-induced K transfer into cells).
- Indications: IV potassium replacement is indicated for following conditions:
- Symptomatic patients with moderate hypokalemia (2.5-3 mEq/L).
- Severe hypokalemia (< 2.5mEq/L) in need of emergent treatment (red flags above)
- Hemodynamically unstable patient e.g. profound shock plus severe hypokalemia (since adequate absorption of potassium via gut is questionable)
- Lack of gut access or function
- Notes
- Potassium is irritating to the endothelium. Adequate dilution is mandatory to prevent pain and phlebitis.
- Potassium can be safely administered through a peripheral IV line at a rate of 10 mEq/h.
- If a more aggressive correction is needed (>20mEq/h), an identical solution can be administered in a second peripheral line (i.e. 10mEq/h through two different peripheral lines). Higher concentrations should be administered through a central line.
- Rate of administration
- Rapid administration of potassium IV can cause transient hyperkalemia with related risk of arrhythmias. Infusion rates should never exceed 20 mEq/h (except in a few conditions, see below).
- Typical rate of potassium administration is as follows.
- 10 mEq/hour: commonly used rate for routine potassium repletion.
- 20 mEq/hr: commonly used for severe hypokalemia or DKA.
- High dose potassium administration may be loosely indicated for certain conditions:
- Cardiac arrest due to hypokalemia (e.g. VT, VF, or asystole): start with 20 mEq potassium IV over 2-3 min 11.
- Recurrent malignant arrhythmias with a pulse: start with 20 mEq potassium IV over 10 min (infusion rate of 60-120 mEq/hr). Down-titrate the rate rapidly as the EKG improves and the patient stabilizes 11 .
- Severe hypokalemia plus (DKA or overdose of beta-blocker/calcium channel blocker)
- Hypokalemia itself isn’t immediately life-threatening here, but hypokalemia impedes the ability to provide insulin (which is needed for the treatment of DKA or for high-dose insulin therapy for poisoning).
- It is reasonable to start infusion of potassium at a rate of 40mEq/hr if the patient is extremely unstable.
- Monitoring serum “K” level
- Serum potassium should initially be measured 2-4 hrs to ascertain the response to therapy. IV regimen should be continued until the serum potassium level is persistently above 3.0 to 3.5 mEq/L and symptoms or signs attributable to hypokalemia have resolved. Thereafter, the dose and frequency or even the route of administration can be reduced to that used in mild to moderate hypokalemia.
Special situation
In patient with severe hypokalemia and volume overload, one may use following preparation
- 10mEq KCl in 100cc half-saline via peripheral line
- 40mEq KCL in 100cc half-saline via central line
Other therapeutic measures
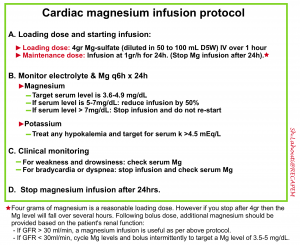
Magnesium repletion
Failure to treat the magnesium deficiency will make it difficult or impossible to fix the hypokalemia (hypomagnesemia causes renal potassium-wasting, so the patient will keep on spilling potassium until their magnesium level is repleted) 4 .
Magnesium repletion is also useful because it will reduce the risk of Torsade de pointes in these patients.
Magnesium can be replaced rapidly (faster than potassium). This may be the fastest approach to decrease the patient’s risk of arrhythmia.
Potassium sparing diuretics
It may be useful in patients with
- Severe volume overload who require ongoing diuretic
- Patients with persistent renal potassium wasting, with inadequate response to potassium supplementation alone
Beta-blockers
When increased sympathetic tone is thought to play a major role in redistributive hypokalemia (e.g. thyrotoxic periodic paralysis, theophylline intoxication, catecholaminergic states), the administration of a nonspecific beta blocker, such as propranolol should be considered.
- In thyrotoxic periodic paralysis, thyroid hormone increases tissue responsiveness to beta-adrenergic stimulation, which, along with thyroid hormone, increases Na/K ATPase activity on the skeletal muscle membrane. This tends to drive potassium into cells, perhaps leading to hyperpolarization of the muscle membrane and relative inexcitability of the muscle fibers 18.
- In such patients, IV propranolol (1mg IV q10min up to total of 3mg) rapidly reverses the hypokalemia and paralysis seen in acute attacks, without rebound hyperkalemia. In another report, propranolol 3 mg/kg “PO”, increased serum potassium and phosphate concentrations in 2 hours with complete resolution of paralysis 19.
Disposition from ED
Discharge
-
Mild hypokalemia.
-
Moderate hypokalemia with minimal symptoms and no other significant risk factors for dysrhythmia and normal QTc.
-
Start repletion of moderate hypokalemic patients in the ED and have close follow-up plan for repeat K.
-
Correct underlying cause, if possible, in all hypokalemic patients.
-
Admission
-
Moderate or severe hypokalemia that cannot rapidly be corrected in the ED.
- Calculate the total-body deficit and decide whether this replacement can reasonably be accomplished in the ED; if not, the patient should be admitted. by enlarge, a serum K decrease by 0.3 mEq/L (below 3.5) represents a total body deficit of 100 mEq.
-
Concerning symptoms associated with hypokalemia, such as paralysis.
-
Significant ECG changes or dysrhythmia.
-
The continued presence of a condition that would promote further potassium loss (e.g, ongoing vomiting or diarrhea).
👉Admission to ICU is considered for patients significant arrhythmia, instability and initial serum K level <2mmol/L.
Further going
References
1. Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. Hypokalemia: a clinical update. Endocr Connect. 2018;7(4):R135-R146. doi:10.1530/EC-18-0109
2. Palmer BF, Clegg DJ. Physiology and Pathophysiology of Potassium Homeostasis: Core Curriculum 2019. Am J Kidney Dis. 2019 Nov;74(5):682-695. doi: 10.1053/j.ajkd.2019.03.427. Epub 2019 Jun 19. PMID: 31227226
3. Skogestad J, Aronsen JM. Hypokalemia-Induced Arrhythmias and Heart Failure: New Insights and Implications for Therapy. Front Physiol. 2018 Nov 7;9:1500. doi: 10.3389/fphys.2018.01500. PMID: 30464746; PMCID: PMC6234658.
4. Ashurst J, Sargent SR, Wagner BJ, Kim J. Evidence-based management of potassium disorders in the emergency department [digest]. Emerg Med Pract. 2016 Nov 22;18(11 Suppl Points & Pearls):S1-S2. PMID: 28745843
5. Chen CT, Wang YC, Lin CM. Hypokalemia-Induced Rhabdomyolysis Caused by Adrenal Tumor-Related Primary Aldosteronism: A Report of 2 Cases. Am J Case Rep. 2021 Apr 10;22:e929758. doi: 10.12659/AJCR.929758. PMID: 33838028; PMCID: PMC8045560
6. Medford-Davis L, Rafique Z. Derangements of potassium. Emerg Med Clin North Am. 2014 May;32(2):329-47. doi: 10.1016/j.emc.2013.12.005. Epub 2014 Feb 28. PMID: 24766936.
7. Levis JT. ECG diagnosis: hypokalemia. Perm J. 2012;16(2):57. doi:10.7812/tpp/12-015
8. Xi H, Yu RH, Wang N, Chen XZ, Zhang WC, Hong T. Serum potassium levels and mortality of patients with acute myocardial infarction: A systematic review and meta-analysis of cohort studies. Eur J Prev Cardiol. 2019 Jan;26(2):145-156. doi: 10.1177/2047487318780466. PMID: 31060369.
9. Skogestad J, Aronsen JM. Hypokalemia-Induced Arrhythmias and Heart Failure: New Insights and Implications for Therapy. Front Physiol. 2018 Nov 7;9:1500. doi: 10.3389/fphys.2018.01500. PMID: 30464746; PMCID: PMC6234658.
10.Veltri KT, Mason C. Medication-induced hypokalemia. P T. 2015 Mar;40(3):185-90. PMID: 25798039; PMCID: PMC4357351.
11.Alfonzo AV, Isles C, Geddes C, Deighan C. Potassium disorders–clinical spectrum and emergency management. Resuscitation. 2006 Jul;70(1):10-25. doi: 10.1016/j.resuscitation.2005.11.002. Epub 2006 Apr 4. PMID: 16600469.
12. Birkhahn RH, Gaeta TJ, Melniker L. Thyrotoxic periodic paralysis and intravenous propranolol in the emergency setting. J Emerg Med. 2000 Feb;18(2):199-202. doi: 10.1016/s0736-4679(99)00194-8. PMID: 10699522
13. Elisaf M, Siamopoulos KC. Fractional excretion of potassium in normal subjects and in patients with hypokalaemia. Postgrad Med J. 1995;71(834):211-212. doi:10.1136/pgmj.71.834.211
14. Blumenfeld JD, Sealey JE, Schlussel Y, Vaughan ED Jr, Sos TA, Atlas SA, Müller FB, Acevedo R, Ulick S, Laragh JH. Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med. 1994 Dec 1;121(11):877-85. doi: 10.7326/0003-4819-121-11-199412010-00010. PMID: 7978702
15. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, Stowasser M, Young WF Jr. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016 May;101(5):1889-916. doi: 10.1210/jc.2015-4061. Epub 2016 Mar 2. PMID: 26934393
16. Choi JS, Kim YA, Kim HY, Oak CY, Kang YU, Kim CS, Bae EH, Ma SK, Ahn YK, Jeong MH, Kim SW. Relation of serum potassium level to long-term outcomes in patients with acute myocardial infarction. Am J Cardiol. 2014 Apr 15;113(8):1285-90. doi: 10.1016/j.amjcard.2014.01.402. Epub 2014 Jan 31. PMID: 24560065
17. Cohn JN, Kowey PR, Whelton PK, Prisant LM. New guidelines for potassium replacement in clinical practice: a contemporary review by the National Council on Potassium in Clinical Practice. Arch Intern Med. 2000 Sep 11;160(16):2429-36. doi: 10.1001/archinte.160.16.2429. PMID: 10979053
18. Rhee EP, Scott JA, Dighe AS. Case records of the Massachusetts General Hospital. Case 4-2012. A 37-year-old man with muscle pain, weakness, and weight loss. N Engl J Med. 2012 Feb 9;366(6):553-60. doi: 10.1056/NEJMcpc1110051. PMID: 22316449
19. Lin SH, Lin YF. Propranolol rapidly reverses paralysis, hypokalemia, and hypophosphatemia in thyrotoxic periodic paralysis. Am J Kidney Dis. 2001 Mar;37(3):620-3. PMID: 11228188





Add comment