5 August 2025, by Abdolghader Pakniyat. Peer-reviewed by Shahriar Lahouti.
Introduction: Setting the Scene
Imagine it’s midnight, and you’re deep into a bustling shift in the Emergency Department (ED). Suddenly, a trauma alert blares overhead: “Code Red, trauma bay two.” Your heart rate spikes, adrenaline surges, and your team rushes into action. Amidst the urgency, noise, and rapid-fire decisions, how do you ensure you’re performing at your best? This is the precise moment where the skill of resuscitation mindfulness becomes indispensable.
Resuscitation mindfulness is not merely a concept—it is a foundational skill combining deliberate focus, emotional regulation, and present-moment awareness to enhance your clinical capabilities during high-stakes scenarios (1).
Why Mindfulness Matters in Emergency Medicine
Emergency medicine is uniquely challenging, marked by high patient acuity, complex decision-making, and intense emotional demands. Even highly experienced clinicians can falter under such pressures, potentially leading to errors or suboptimal care (2). Mindfulness serves as an anchor, stabilizing cognitive and emotional responses, ultimately enhancing patient outcomes and promoting physician well-being.
Scenario-Based Exploration: A Case in the ED
Consider this clinical vignette: A 55-year-old patient arrives unconscious with unstable vital signs after a motor vehicle collision. Multiple injuries are evident, and your team immediately initiates resuscitation. As the attending physician, you face immense pressure—rapid interventions are required. Here is where mindfulness makes a critical difference:
Step 1: Focused Attention Amid Chaos
In such scenarios, distractions abound: alarms blare, multiple people speak simultaneously, and the patient’s condition evolves rapidly. Mindfulness sharpens your ability to sustain attention on critical tasks—like managing the airway or monitoring hemodynamics—while filtering out extraneous noise and anxiety (1).
- Practical Exercise: Use brief “anchoring breaths”—two deep, deliberate breaths before each major intervention—to maintain clarity and composure.
Step 2: Cultivating Present-Moment Awareness
Mindfulness emphasizes engaging directly with what is happening right now. Rather than becoming overwhelmed by future worries (“Will this patient survive?”) or past errors (“I should have intubated earlier”), mindfulness helps you remain fully present. This sharpens your situational awareness, helping you accurately interpret clinical data and make precise, timely decisions (3).
- Practical Exercise: Practice a quick mental checklist: “Right now, what do I see, hear, and feel?” to ground yourself.
Step 3: Non-Judgmental Observation and Emotional Balance
Resuscitations often evoke intense emotions like anxiety, frustration, or self-criticism. Mindfulness teaches recognizing these emotions without immediate reaction, allowing for better emotional management. This skill is crucial as emotional stability directly influences clinical decision-making and team dynamics (2).
- Practical Exercise: Briefly acknowledge your internal state (“I’m feeling tense”), without judgment, then consciously refocus on the clinical task at hand.
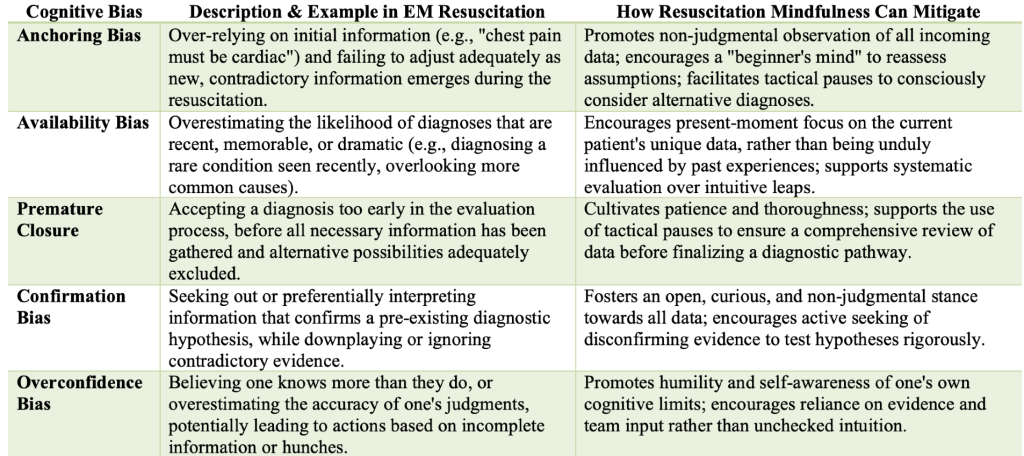
Step 4: Navigating Cognitive Pitfalls with Mindfulness
In high-stakes resuscitations, physicians are vulnerable to cognitive biases (6):
Step 5: Post-Resuscitation Reflection
Following the intensity of a resuscitation, structured reflection is vital. Mindfulness fosters structured debriefing and personal reflection, facilitating emotional processing, identifying learning points, and reinforcing resilience (5).
- Practical Exercise: After stabilization, lead a structured team debrief using the PEARLS method: outline what went well, areas for improvement, and key emotional takeaways.
Conclusion: Embracing Mindfulness in Emergency Medicine
Mindfulness is more than an ancillary skill; it’s a critical foundational competency in emergency medicine. It enhances clinical effectiveness, improves team communication, reduces cognitive errors, and supports physician well-being. By integrating mindfulness into your daily practice, you empower yourself to navigate the demanding and dynamic environment of emergency care with greater clarity, resilience, and effectiveness (4).
References
1. Mindfulness and the Emergency Medicine Mind. Retrieved from: https://www.emra.org/books/emra-wellness-guide/ch1.-mindfulness-and-the-emergency-medicine-mind
2. Performance Under Pressure. Retrieved from: https://first10em.com/performance-under-pressure/
3. Emergency Medicine Milestones. Retrieved from: https://www.acgme.org/globalassets/pdfs/milestones/emergencymedicinesupplementalguide.pdf
4. PMC. (2025). Cognitive biases in diagnosis. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8520040/
5. Greater Good Science Center. (2025). What We Can Learn from a Mindful Emergency Room. Retrieved from: https://greatergood.berkeley.edu/article/item/what_we_can_learn_from_a_mindful_emergency_room
6. Cognitive biases in diagnosis and decision making during anaesthesia and intensive care, accessed June 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8520040/


Add comment