29. September 2021, via Shahriar Lahouti
CONTENTS
- Preface
- Pathogenesis
- Microbiology
- Clinical manifestation
- Diagnosis
- Differential diagnosis
- Approach to diagnosis and management
- Initial assessment
- Algorithm
- Recent evidence for therapeutic options
- Non-severe bronchiolitis
- Severe bronchiolitis
- Admission criteria
- Discharge criteria
- Education and follow up
- Appendix
- References
Preface
Bronchiolitis is a lower respiratory tract infection that primarily affects the small airways (bronchioles). It typically affects infants and children younger than two years, principally during the fall and winter. In this post, recent evidence regarding management of bronchiolitis is explored.
Pathogenesis
Bronchiolitis occurs when viruses infect the terminal bronchiolar epithelial cells, causing direct damage and inflammation in the small bronchi and bronchioles. Edema, excessive mucus, and sloughed epithelial cells lead to obstruction of small airways and atelectasis.
Microbiology
RSV is the most common culprit, followed by rhinovirus. Other potential pathogen include
- Parainfluenza virus
- Human metapneumovirus
- Influenza virus
- Adenovirus
- Coronavirus
- Human bocavirus
Clinical manifestation
A clinical syndrome of respiratory distress that occurs typically in children <2 years of age and presents with symptoms of a viral URI e.g. rhinorrhea, congestion, cough and fever (usually ≤ 38.3°C) and post-tussive vomiting, in an infant progressing to lower respiratory involvement evidenced by a constellation of these findings 1 :
- ↑Work of breathing
- Retraction
- Tachypnea
- Impaired Oxygenation
- Wheeze
- Coarse rales
👉Remember that respiratory distress, increased work of breathing, respiratory rate, and oxygenation all can change rapidly with crying, coughing, and agitation.
Risk factor for severe disease
- Prematurity (gestational age ≤36 weeks)
- Low birth weight
- Age less than 12 weeks
- Chronic pulmonary disease, particularly bronchopulmonary dysplasia (also known as chronic lung disease)
- Anatomic defects of the airways
- Hemodynamically significant congenital heart disease
- Immunodeficiency
- Neurologic disease
Environmental and other risk factors, such as passive smoking, crowded household, daycare attendance, being born approximately two months before or after the start of the epidemic, concurrent birth siblings, older siblings, and high altitude (>2500 meters), can also contribute to more severe disease.
Typical illness with bronchiolitis begins with upper respiratory tract symptoms, followed by lower respiratory tract signs and symptoms on days 2 to 3, which peak on days 3 to 5 and then gradually resolve. The duration of the illness due to bronchiolitis depends upon age, severity of illness, associated high-risk conditions (eg, prematurity, chronic pulmonary disease), and the causative agent.
In most previously healthy infants, bronchiolitis resolves without complications. Possible associated complications especially in high risk group include
👉Apnea: The overall incidence of apnea in bronchiolitis is 2.7% but in those under 6 weeks of age, the risk can be as high as 5%. Risk factors that are associated with apnea in patients with Bronchiolitis include:
- Small for gestational age < 5 (2.3 kg)
- Age < 2 months
- Oxygen saturations < 90%
- Previous episode of apnea
Diagnosis
Bronchiolitis is a clinical diagnosis.The evaluation of infants and young children with suspected bronchiolitis generally requires only history and physical examination, including pulse oximetry.
History
Typical features include a viral upper respiratory prodrome followed by increased respiratory effort (eg, tachypnea, nasal flaring, chest retractions) and wheezing and/or crackles in children younger than two years of age.
Examination
Assessment is ideally done with the child upright, awake after suctioning the upper airway, as nasal congestion may transmit to the lungs and simulate wheezing.
Typical findings of bronchiolitis include tachypnea, intercostal and subcostal retractions, expiratory wheezing, and cough.
Additional auscultatory findings may include prolonged expiratory phase and rales (coarse or fine). Hypoxemia (oxygen saturation <95%) commonly is detected by pulse oximetry.
Other findings may include conjunctivitis, pharyngitis, and acute otitis media 6.
👉Findings in severely affected patients include
- ↑work of breathing (subcostal, intercostal, and supraclavicular retractions; nasal flaring; and expiratory grunting)
- Cyanosis
- Poor peripheral perfusion
👉Wheezing may not be audible if the airways are profoundly narrowed or when increased work of breathing results in exhaustion.
Assessing severity of the disease
Features which help to identifying severity of illness and hospitalization should be sought including:
- Assessment of hydration status (eg, fluid intake, urine output)
- Symptoms of respiratory distress (tachypnea, nasal flaring, retractions, grunting)
- Cyanosis
- Episodes of restlessness or lethargy (may indicate hypoxemia and/or impending respiratory failure)
- A history of apnea with or without cyanosis or bradycardia
- Past medical history: Features associated with severe disease include prematurity, chronic pulmonary disease, anatomic abnormalities of the airways, hemodynamically significant congenital heart disease, immunodeficiency, and neurologic disease.
Laboratory studies and radiographs usually are not necessary for diagnosis but may be warranted to evaluate complications, comorbid infections, or other conditions in the differential diagnosis 7.
Chest radiographs are not necessary in the routine evaluation of bronchiolitis 8 and they should be obtained only if there are clinical findings suggestive of other potential diagnoses. Consider CXR if:
- Clinical picture is not consistent with typical bronchiolitis
- Clinical course suggests super infection
- New fever late in the disease process
- Severe disease / toxic appearance with a lack of upper respiratory symptoms
Radiographic features of bronchiolitis, which are variable and nonspecific, include hyperinflation and peribronchial thickening. Patchy atelectasis with volume loss may result from airway narrowing and mucus plugging 9
👉In the following conditions extensive laboratory testing may be warranted:
- Neonates or Infants (29-90 days of age) with fever and signs and symptoms of bronchiolitis who appear toxic, have signs / symptoms of UTI or have risk factors for serious bacterial infection. In this situation a CBC, Blood culture and/or urinalysis and urine culture may be warranted to exclude comorbid or secondary bacterial infection.
- In children of any age with unusual or severe course extensive work up (e.g. CBC, cultures, urinalysis) may be warranted.
Differential diagnosis
Bronchiolitis must be distinguished from a variety of acute and chronic conditions that affect the respiratory tract. The differential diagnosis include:
👉Recurrent viral-triggered wheezing or asthma: is a major consideration in the differential diagnosis of bronchiolitis in older infants and toddlers. Helpful features in favor of asthma may include:
- A history of recurrent wheezing episodes and a family or personal history of asthma, eczema, and atopy (however, during the first episode of wheezing, it is difficult to distinguish bronchiolitis from asthma) 10
- Prior bronchodilator or corticosteroid use
- Age > 12 months
- Strong response to albuterol
👉Bacterial pneumonia: It may be difficult to differentiate bronchiolitis from bacterial pneumonia in young children. Findings that may suggest bacterial pneumonia include: 11 12
- Toxic appearance
- Abrupt onset
- Fever late in the course of illness
- Chills
- WBC count >15,000/microL (if obtained)
- Elevated acute phase reactants (if obtained)
- CXR: Consolidation (lobar or segmental), alveolar infiltrate
👉Pertussis: Should be suspected in infants and young children. Helpful clues may include 13 14 15
- Usually absence of significant fever
- Prolonged cough that is not improving (note that cough may or may not be paroxysmal; with or without a whoop or posttussive vomiting)
- A cough illness associated with rhinorrhea in which the nasal discharge remains watery
- Leukocytosis with lymphocytosis (WBC ≥20,000 cells/microL with ≥50% lymphocytes)
- Apnea, seizures, cyanosis, vomiting, or poor weight gain
- Known pertussis exposure
👉Chronic pulmonary disease: Chronic underlying pulmonary conditions should be suspected in children with prolonged or recurrent symptoms, such as recurrent wheezing, poor weight gain, recurrent aspiration, stridor, or recurrent respiratory infection. The clinical course of bronchiolitis in children with underlying pulmonary disorders tends to be severe and may require prolonged hospitalization.
👉Foreign body aspiration: Clinical features of foreign body aspiration may include
- A history of choking (may not always present)
- Focal monophonic wheezing
- Decreased air entry
- A high index of suspicion should be maintained for foreign body aspiration so that definitive treatment can be provided.
👉Aspiration pneumonia: Aspiration pneumonia may occur secondary to gastroesophageal reflux disease and/or swallowing dysfunction. It also may occur as a complication of bronchiolitis; the risk of aspiration increases during active bronchiolitis and resolves weeks later as tachypnea and the work of breathing subside. Clinical features associated with aspiration may include coughing with feeds, weak suck reflex, cyanosis during feeding, and recurrent or chronic stridor.
👉Congenital heart disease, heart failure: Associated clinical findings of heart failure in infants may include easy fatigue and/or diaphoresis with feeding, poor weight gain, poor peripheral perfusion, and abnormalities on cardiac examination and hepatomegaly
👉Vascular ring: Although stridor is more common, children with vascular rings may also have wheezing (typically with pulmonary artery slings). Imaging including lateral chest radiography (anterior bowing of the trachea) , barium contrast esophagogram, bronchoscopy, magnetic resonance angiography) usually are necessary for definitive diagnosis.
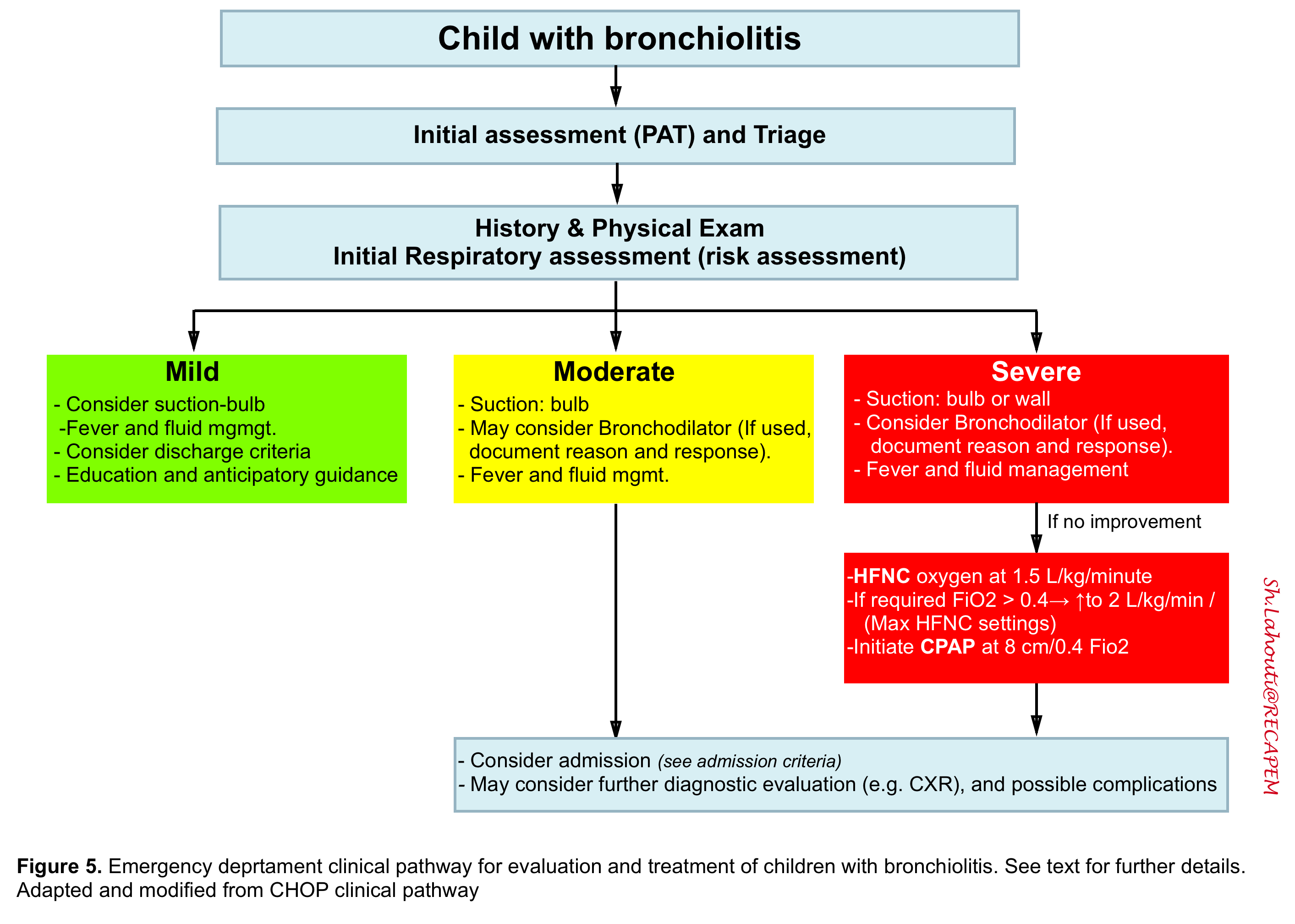
Approach to diagnosis and management
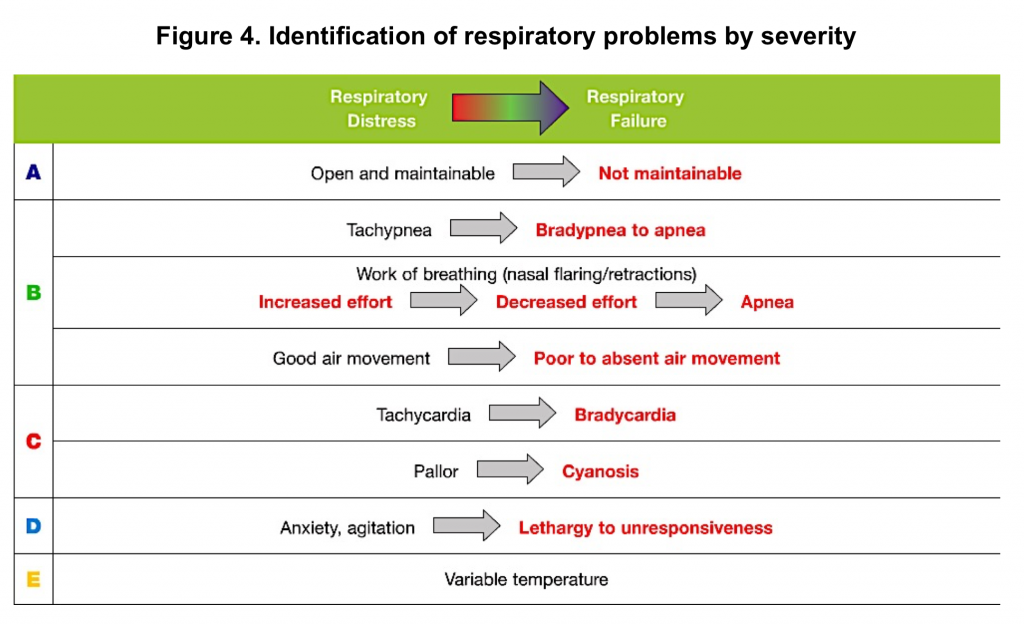
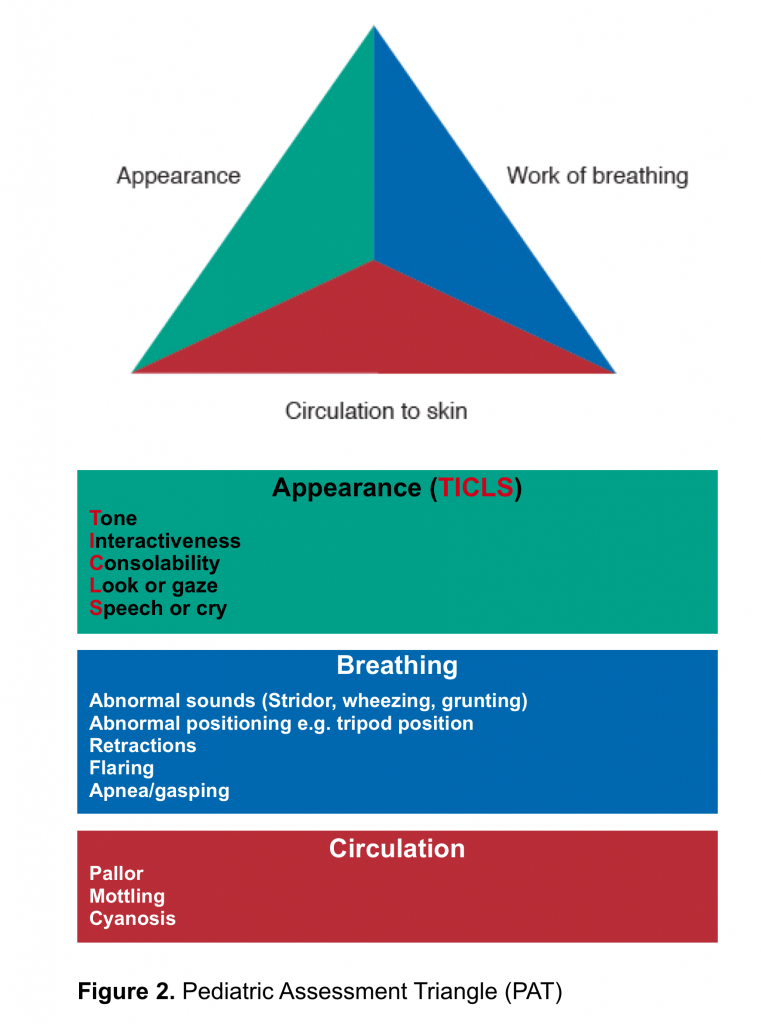
The initial evaluation of a sick child involves rapid assessment (via pediatric assessment triangle; PAT) shown in the following figure (figure 2). The normal limits of pediatric vitals is presented in figure 3.
👉Upper limit of normal respiratory rate by age can be memorized as:
- Term Newborn 50 breaths/minute
- 6 months 40 breaths/minute
- 12 months 30 breaths/minute
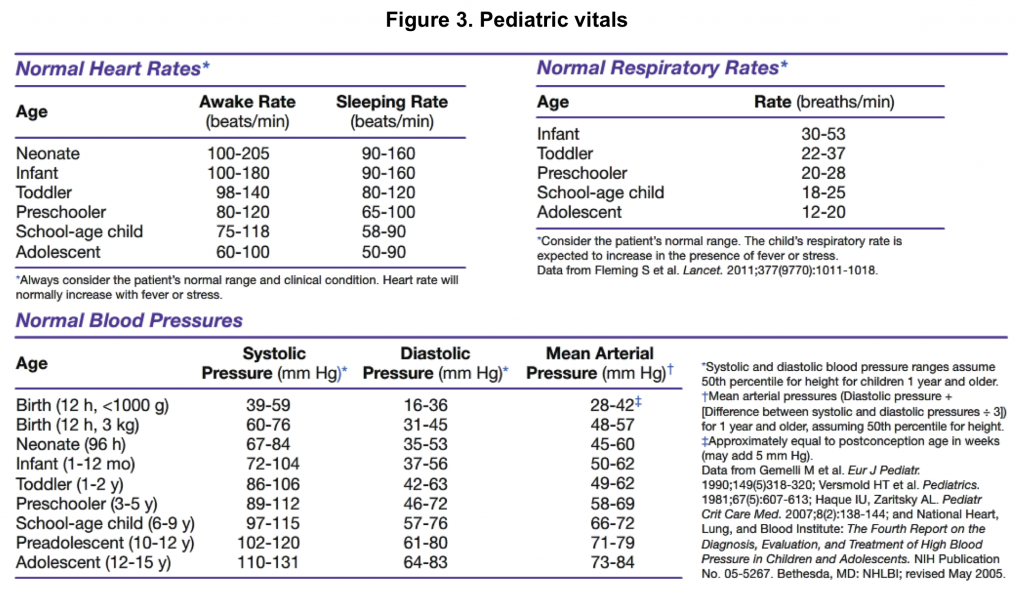
Upon appropriate initial assessment and triage (more on this here), prompt resuscitation is performed accordingly (discussed separately). Oftentimes, the severity of respiratory problems can be classified (figure 4).
The general management strategy for respiratory emergency involve:
- Head positioning
- Suctioning
- Oxygen
- Access
Subsequent management depends on a constellation of data obtained by history and physical examination (appendix 1). In this post, the management strategies for bronchiolitis is explored.
The following approach is consistent with that of the American Academy of Pediatrics, the National Institute for Care Excellence, and other professional organizations.
Schema of diagnostic and therapeutic approach to bronchiolitis is represented below (figure 5).
Recent evidence for possible therapeutic Options
Nasal suctioning in bronchiolitis
In a retrospective cohort study of 740 infants (2 to 12 months) hospitalized with bronchiolitis, those who had three or four lapses of mechanical suctioning of more than four hours had longer hospital stay than those who had no lapses in suctioning (2.64 versus 1.62 days)16
- There is little evidence to support routine frequent “deep” suctioning of the oropharynx or larynx with a nasopharyngeal catheter. Catheter suctioning of the nasopharynx is traumatic and may produce edema and nasal obstruction. Catheter suctioning of the oropharynx can induce cough, but the theoretic complication of laryngospasm is not corroborated.
Given that infants are obligate nasal breathers until 2 months of age and the upper airway obstruction from mucus can contribute significantly to the patient’s breathing difficulties, a trial of nasal suctioning is not unreasonable in the ED.
For children hospitalized with bronchiolitis, mechanical aspiration of the nares as necessary to relieve nasal obstruction. Saline nose drops and mechanical aspiration of nares may help to relieve partial upper airway obstruction in infants and young children with respiratory distress or feeding difficulties.
Bronchodilators (inhaled or oral)
There’s no evidence of benefit for bronchodilators in bronchiolitis 17 18.
A trial of salbutamol may be considered for patients in whom there is a strong family history of asthma, atopy, or in the patient who has had multiple wheezing episodes.
Approximately 15-25% of infants with bronchiolitis will respond to bronchodilators. If a trial of salbutamol is going to be attempted, the clinician should objectively assess the work of breathing before and after its administration (more on this here) and continue therapy only if a clinical benefit is noted.
A Cochrane Review from 2011 found that nebulized epinephrine reduced admission rates on day 1, however there was no difference in hospitalization within 7 days compared to placebo. Clinical severity scores have been shown to be significantly decreased at 60 and 120 mins after administration of nebulized epinephrine compared with placebo, but this effect is not prolonged. Thus, epinephrine may provide short-term benefit only and may only temporarily delay the need for admission. Nebulized epinephrine or salbutamol may be considered in patients in whom you suspect admission will be the likely disposition. You must monitor the patient objectively for the benefit of treatment to guide further management.
Glucocorticoid (inhaled, oral)
In randomized trials and meta-analysis, inhaled glucocorticoids (budesonide, fluticasone, dexamethasone) have not been beneficial in reducing symptom duration or readmission rates 19 and it’s not routinely recommended.
There is little evidence to support the benefit of adjunctive glucocorticoids in the management of respiratory failure due to bronchiolitis. A meta-analysis of three studies evaluating the use of systemic glucocorticoids in infants with bronchiolitis requiring admission to the ICU did not find an effect on duration of mechanical ventilation or length of hospitalization 20
Bronchodilators plus glucocorticoids
Although a randomized trial suggested that administration of nebulized epinephrine and oral dexamethasone in the emergency department decreased the rate of hospitalization within one week of the emergency department visit 21, the result was not significant when adjusted for multiple comparisons.
Nebulized hypertonic saline
Hypertonic saline is theorized to be of benefit based on its ability to reduce airway edema and mucous plugging, however there’s no solid evidence for routine use in bronchiolitis. It can be considered as a temporizing measure for a patient who is going to be admitted and not as a rescue maneuver.
In a 2018 meta-analysis of eight randomized trials evaluating administration of hypertonic saline in the ED, hypertonic saline reduced the rate of hospitalization among children with bronchiolitis (risk ratio 0.77, 95% CI 0.62-0.96), but there was substantial heterogeneity 22 23
The 2014 AAP clinical practice guideline on the management of bronchiolitis indicated that clinicians “may administer hypertonic saline to infants and children hospitalized for bronchiolitis”.
Supplemental oxygen
Supplemental oxygen should be provided by nasal cannula, face mask, or head box to maintain SO2 above 90 to 92%.24
Data are lacking to support the use of a specific SO2 cutoff value. The American Academy of Pediatrics practice guideline suggests SO2 < 90% as the threshold to start supplemental oxygen.
👉Close monitoring is required as supplemental oxygen is weaned, particularly for children with hemodynamically significant heart disease, bronchopulmonary dysplasia, and premature birth.
Although standard oxygen therapy is effective for the majority of children with bronchiolitis who require supplemental oxygen; heated humidified high-flow nasal cannula (HFNC, also called high-flow warm humidified oxygen) therapy and/or continuous positive airway pressure (CPAP) are used to reduce the work of breathing, improve gas exchange, and avoid endotracheal intubation in children with bronchiolitis who are at risk for progression to respiratory failure.
High-flow warm humidified oxygen
In observational studies, HFNC has been associated with decreased rates of endotracheal intubation 25 . Although this benefit has not been proven in randomized trials, HFNC may avoid the need for endotracheal intubation and is better tolerated and has fewer adverse effects than CPAP 26
HFNC is a well-tolerated noninvasive method of ventilatory support that permits high inspired gas flows (4 to 8 L/min) with or without increased oxygen concentration. The increased flows are tolerated because the air is humidified.
Flow rates ≥6 L/min can generate positive expiratory pressures in the range of 2 to 5 cm H2O. The size of the nasal cannula, which is determined by fit, affects the size of the circuit and maximum amount of flow. For the treatment of bronchiolitis in infants and children younger than two years, 8 L/min is generally the maximum flow rate, but higher rates may be used (cannula size permitting) 27
While this modality may not be tolerated by all patients, in those who are showing signs of fatigue and in whom you are considering intubation, there may be a role for high flow oxygen.
While ketamine is an option in these patients, it is not recommended, unless it is going to be used in RSI. While it may have benefits in asthmatic patients due to its bronchodilatory properties, bronchoconstriction is not thought to play a significant role in bronchiolitis and thus ketamine is unlikely to be of benefit. In addition, ketamine may increase secretions in high doses, which may further worsen oxygenation in this group of patients.
Contraindications to HFNC include
- Abnormalities of the face or airway that preclude an appropriate-fitting nasal cannula 28.
- Relative contraindications include confusion or agitation, vomiting, excessive secretions, and bowel obstruction.
Complications of HFNC include abdominal distension, aspiration, barotrauma, and pneumothorax (rare).
👉Infants receiving HFNC who are clinically deteriorating may develop significant respiratory acidosis (hypercapnia) despite high oxygen saturations (if they are receiving supplemental O2). Oxygen saturation is a poor indicator of impending respiratory failure, which is better indicated by marked retractions, decreased or absent breath sounds, fatigue, and poor responsiveness to stimulation (eg, weak or no cry).
- Blood gas analysis to assess ventilation (ie, PCO2 levels) may be warranted in infants receiving HFNC who become more dyspneic and/or tachycardic.
CPAP
It can be used to avoid endotracheal intubation in infants and children with bronchiolitis who have failed standard oxygen therapy and are at risk for respiratory failure (eg, persistently increased respiratory effort, hypoxemia). CPAP can decrease work of breathing and prevent endotracheal intubation in children with progressive hypoxemia or hypercarbia.
Endotracheal intubation
Infants who have ongoing or worsening severe distress despite a trial of HFNC and/or CPAP, those who have hypoxemia despite oxygen supplementation, and those with apnea may require endotracheal intubation and mechanical ventilation.
Signs of impending respiratory failure in infants and young children with bronchiolitis include marked retractions, decreased or absent breath sounds, fatigue, and poor responsiveness to stimulation (eg, weak or no cry).
Arterial or venous blood gases obtained in infants with impending respiratory failure often reveal hypercapnia (i.e. PCO2 >55 mmHg [arterial sample] or >60 mmHg [venous sample]); however, blood gases should not be used as the sole basis for deciding to intubate.
Antibiotic agents / immunotherapies
Antibiotic: Not recommended for bronchiolitis. If concomitant or secondary bacterial infection is present, it is treated in the same manner as it would be in the absence of bronchiolitis.
Ribavirin: May be considered for severe bronchiolitis in immunocompromised patients
Immunotherapies: Intravenous immunoglobulin with a high neutralizing activity against RSV (RSV-IGIV, which has been discontinued) and RSV-specific humanized monoclonal antibody (palivizumab) failed to improve outcomes in infants (with or without risk factors) hospitalized with RSV infection 29.
Non-severe bronchiolitis
Can be managed in an outpatient setting, unless there are concerns about the caregivers’ ability to care for them at home.
Pharmacologic interventions are not recommended because they lack proven benefit, increase the cost of care, and may have adverse effects. Recent studies do not support the benefits of bronchodilators 16 (inhaled or oral) , glucocorticoids (inhaled or systemic). Antibiotics are indicated only if there is evidence of a coexisting bacterial infection.
For infants and children with non-severe bronchiolitis who are treated in the office or emergency department, nebulized hypertonic saline is not routinely recommended.
Severe bronchiolitis
Possible therapeutic consideration include:
- Nasal suction
- 3% hypertonic saline nebulization
- Inhaled bronchodilator: Although routine use of bronchodilator is not recommended, a one-time trial of inhaled bronchodilators (salbutamol or epinephrine) may be warranted for infants and children with bronchiolitis and severe disease (i.e. persistently increased respiratory effort [tachypnea, nasal flaring, retractions, accessory muscle use, grunting], hypoxemia, apnea, or respiratory failure).
- Albuterol: 0.15 mg/kg (minimum 2.5 mg; maximum 5 mg) diluted in 2.5mL normal saline and administered over 5 to 15 minutes or four to six puffs via a metered dose inhaler with spacer and face mask. The effects should be monitored by evaluating the child before and up to one hour after treatment.
- HFNC / CPAP (see above)
Monitoring clinical status
- Respiratory status: repeated clinical assessment of the respiratory system (eg, respiratory rate, nasal flaring, retractions, grunting) is necessary to identify deteriorating respiratory status
- Fluid status: children with bronchiolitis may have difficulty maintaining adequate hydration because of increased needs related to fever and tachypnea and decreased intake related to tachypnea and respiratory distress.
- The fluid intake and output of infants and children with bronchiolitis should be assessed regularly.
- For children who can tolerate enteral feedings, strategies to maintain hydration include small frequent feedings or orogastric or nasogastric feedings.
- Exclusive parenteral fluid administration may be necessary to ensure adequate hydration and avoid the risk of aspiration in infants and children who are hospitalized with bronchiolitis and have moderate to severe respiratory distress.
- It is also important to monitor urine output. Plasma antidiuretic hormone levels rarely may be elevated, leading to fluid retention and hyponatremia 30. Fluid overload should be avoided, since it may lead to pulmonary congestion and worse outcomes.
- The fluid intake and output of infants and children with bronchiolitis should be assessed regularly.
Admission criteria
The criteria for admission 31 may include:
- Apnea
- Signs of severe respiratory distress (indrawing, grunting, RR>70)
- Supplemental O2 required to keep saturations >90%
- Dehydration or history of poor fluid intake
- Cyanosis or history of apnea
- Infant at high risk for severe disease (see above)
- Family unable to cope
Discharge criteria
Minimal clinical criteria for discharge from the hospital or emergency department include 32
- Respiratory rate <60 breaths per minute for age <6 months, <55 breaths per minute for age 6 to 11 months, and <45 breaths per minute for age ≥12 months
- Caretaker knows how to clear the infant’s airway using bulb suctioning
- Patient is stable while breathing ambient air; discharge from the hospital requires that the patient remain stable for at least 12 hours prior to discharge
- Patient has adequate oral intake to prevent dehydration
- Resources at home are adequate to support the use of any necessary home therapies (eg, bronchodilator therapy if the trial was successful and this therapy is to be continued)
- Caretakers are confident they can provide care at home
- Education of the family is complete
Remember that bronchiolitis symptoms peak around days 3-5. If the patient presents on Day 2, you can expect the patient may get worse before they get better. This should be factored into your disposition decision. Also, 50% of patients who develop severe disease do so after their first ED visit, so clear discharge instructions are very important.
Education and Follow-up
Education and anticipatory guidance are important aspects of the management of bronchiolitis. Components of education and anticipatory guidance include:
- Expected clinical course: Typical illness with bronchiolitis begins with upper respiratory tract symptoms. Lower respiratory symptoms and signs develop on days 2 to 3, peak on days 3 to 5, and then gradually resolve over the course of two to three weeks.
- Proper techniques for suctioning the nose (more on this here)
- Avoidance of over-the-counter decongestants and cough medicines
- Indications to return to medical care immediately: apnea, cyanosis, poor feeding, new fever, increased respiratory rate and/or increased work of breathing (retractions, nasal flaring, grunting), decreasing fluid intake (<75% of normal, no wet diaper for 12 hours), exhaustion (eg, failure to respond to social cues, waking only with prolonged stimulation)
- The need to monitor fluid intake and output: children with bronchiolitis may have difficulty maintaining adequate hydration because of increased needs (related to fever and tachypnea) and decreased intake (related to tachypnea and respiratory distress).
Children with bronchiolitis who are not hospitalized should be monitored by their clinician for progression and resolution of disease. Follow-up, usually within one to two days, may occur by phone or at the office. The timing and method of follow-up depend upon initial severity and duration of symptoms; patients who are seen in the first one to two day of symptoms may worsen before they improve.
In children who do not improve as expected, CXR and/or extended blood work may be helpful in excluding other conditions in the differential diagnosis (see above).
Appendix 1
References
1. Florin TA, Plint AC, Zorc JJ. Viral bronchiolitis. Lancet. 2017 Jan 14;389(10065):211-224. doi: 10.1016/S0140-6736(16)30951-5. Epub 2016 Aug 20. PMID: 27549684; PMCID: PMC6765220.
2. Schroeder AR, Mansbach JM, Stevenson M, Macias CG, Fisher ES, Barcega B, Sullivan AF, Espinola JA, Piedra PA, Camargo CA Jr. Apnea in children hospitalized with bronchiolitis. Pediatrics. 2013 Nov;132(5):e1194-201. doi: 10.1542/peds.2013-1501. Epub 2013 Oct 7. PMID: 24101759; PMCID: PMC3813402
3. Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr. Trends in bronchiolitis hospitalizations in the United States, 2000-2009. Pediatrics. 2013 Jul;132(1):28-36. doi: 10.1542/peds.2012-3877. Epub 2013 Jun 3. PMID: 23733801; PMCID: PMC3691534
4. Hall CB, Powell KR, Schnabel KC, Gala CL, Pincus PH. Risk of secondary bacterial infection in infants hospitalized with respiratory syncytial viral infection. J Pediatr. 1988 Aug;113(2):266-71. PMID: 3397789
5. Pinnington LL, Smith CM, Ellis RE, Morton RE. Feeding efficiency and respiratory integration in infants with acute viral bronchiolitis. J Pediatr. 2000 Oct;137(4):523-6. doi: 10.1067/mpd.2000.108396. PMID: 11035832
6. Shazberg G, Revel-Vilk S, Shoseyov D, Ben-Ami A, Klar A, Hurvitz H. The clinical course of bronchiolitis associated with acute otitis media. Arch Dis Child. 2000 Oct;83(4):317-9. doi: 10.1136/adc.83.4.317. PMID: 10999866; PMCID: PMC1718509
7. Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Bailey JE, Gadomski AM, Johnson DW, Light MJ, Maraqa NF, Mendonca EA, Phelan KJ, Zorc JJ, Stanko-Lopp D, Brown MA, Nathanson I, Rosenblum E, Sayles S 3rd, Hernández-Cancio S; American Academy of Pediatrics. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014 Nov;134(5):e1474-502. doi: 10.1542/peds.2014-2742. Erratum in: Pediatrics. 2015 Oct;136(4):782. PMID: 25349312
8. Bordley WC, Viswanathan M, King VJ, Sutton SF, Jackman AM, Sterling L, Lohr KN. Diagnosis and testing in bronchiolitis: a systematic review. Arch Pediatr Adolesc Med. 2004 Feb;158(2):119-26. doi: 10.1001/archpedi.158.2.119. PMID: 14757603
9. Dawson KP, Long A, Kennedy J, Mogridge N. The chest radiograph in acute bronchiolitis. J Paediatr Child Health. 1990 Aug;26(4):209-11. doi: 10.1111/j.1440-1754.1990.tb02431.x. PMID: 2257182.
10. Landau LI. Bronchiolitis and asthma: are they related? Thorax. 1994 Apr;49(4):293-6. doi: 10.1136/thx.49.4.293. PMID: 8202895; PMCID: PMC475358.
11. Murphy CG, van de Pol AC, Harper MB, Bachur RG. Clinical predictors of occult pneumonia in the febrile child. Acad Emerg Med. 2007 Mar;14(3):243-9. doi: 10.1197/j.aem.2006.08.022. Epub 2007 Jan 22. PMID: 17242382
12. Harris M, Clark J, Coote N, Fletcher P, Harnden A, McKean M, Thomson A; British Thoracic Society Standards of Care Committee. British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011 Oct;66 Suppl 2:ii1-23. doi: 10.1136/thoraxjnl-2011-200598. PMID: 21903691
13. Cherry JD, Tan T, Wirsing von König CH, Forsyth KD, Thisyakorn U, Greenberg D, Johnson D, Marchant C, Plotkin S. Clinical definitions of pertussis: Summary of a Global Pertussis Initiative roundtable meeting, February 2011. Clin Infect Dis. 2012 Jun;54(12):1756-64. doi: 10.1093/cid/cis302. Epub 2012 Mar 19. PMID: 22431797; PMCID: PMC3357482
14. Cherry JD, Wendorf K, Bregman B, Lehman D, Nieves D, Bradley JS, Mason WH, Sande-Lopez L, Lopez M, Federman M, Chen T, Blumberg D, Johnston S, Schwenk HT, Weintrub P, Quinn KK, Winter K, Harriman K. An Observational Study of Severe Pertussis in 100 Infants ≤120 Days of Age. Pediatr Infect Dis J. 2018 Mar;37(3):202-205. doi: 10.1097/INF.0000000000001710. PMID: 28737623.
15. Centers for Disease Control and Prevention. Pertussis (whooping cough). Surveillance & Reporting. http://www.cdc.gov/pertussis/surv-reporting.html (Accessed on November 30, 2020).
16. Mussman GM, Parker MW, Statile A, Sucharew H, Brady PW. Suctioning and length of stay in infants hospitalized with bronchiolitis. JAMA Pediatr. 2013 May;167(5):414-21. doi: 10.1001/jamapediatrics.2013.36. PMID: 23460088; PMCID: PMC6291830.
17. Skjerven HO, Hunderi JO, Brügmann-Pieper SK, Brun AC, Engen H, Eskedal L, Haavaldsen M, Kvenshagen B, Lunde J, Rolfsjord LB, Siva C, Vikin T, Mowinckel P, Carlsen KH, Lødrup Carlsen KC. Racemic adrenaline and inhalation strategies in acute bronchiolitis. N Engl J Med. 2013 Jun 13;368(24):2286-93. doi: 10.1056/NEJMoa1301839. PMID: 23758233
18. Gadomski AM, Scribani MB. Bronchodilators for bronchiolitis. Cochrane Database Syst Rev. 2014 Jun 17;2014(6):CD001266. doi: 10.1002/14651858.CD001266.pub4. PMID: 24937099; PMCID: PMC7055016
19. Fernandes RM, Bialy LM, Vandermeer B, Tjosvold L, Plint AC, Patel H, Johnson DW, Klassen TP, Hartling L. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev. 2013 Jun 4;2013(6):CD004878. doi: 10.1002/14651858.CD004878.pub4. PMID: 23733383; PMCID: PMC6956441
20. Davison C, Ventre KM, Luchetti M, Randolph AG. Efficacy of interventions for bronchiolitis in critically ill infants: a systematic review and meta-analysis. Pediatr Crit Care Med. 2004 Sep;5(5):482-9. doi: 10.1097/01.pcc.0000128891.54799.67. PMID: 15329166; PMCID: PMC3867796
21. Plint AC, Johnson DW, Patel H, Wiebe N, Correll R, Brant R, Mitton C, Gouin S, Bhatt M, Joubert G, Black KJ, Turner T, Whitehouse S, Klassen TP; Pediatric Emergency Research Canada (PERC). Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med. 2009 May 14;360(20):2079-89. doi: 10.1056/NEJMoa0900544. PMID: 19439742
22. Heikkilä P, Renko M, Korppi M. Hypertonic saline inhalations in bronchiolitis-A cumulative meta-analysis. Pediatr Pulmonol. 2018 Feb;53(2):233-242. doi: 10.1002/ppul.23928. Epub 2017 Dec 21. PMID: 29266869
23. Brooks CG, Harrison WN, Ralston SL. Association Between Hypertonic Saline and Hospital Length of Stay in Acute Viral Bronchiolitis: A Reanalysis of 2 Meta-analyses. JAMA Pediatr. 2016 Jun 1;170(6):577-84. doi: 10.1001/jamapediatrics.2016.0079. PMID: 27088767
24. Panitch HB. Respiratory syncytial virus bronchiolitis: supportive care and therapies designed to overcome airway obstruction. Pediatr Infect Dis J. 2003 Feb;22(2 Suppl):S83-7; discussion S87-8. doi: 10.1097/01.inf.0000053890.66801.97. PMID: 12671457.
25. Wing R, James C, Maranda LS, Armsby CC. Use of high-flow nasal cannula support in the emergency department reduces the need for intubation in pediatric acute respiratory insufficiency. Pediatr Emerg Care. 2012 Nov;28(11):1117-23. doi: 10.1097/PEC.0b013e31827122a9. PMID: 23114231
26. Milési C, Essouri S, Pouyau R, Liet JM, Afanetti M, Portefaix A, Baleine J, Durand S, Combes C, Douillard A, Cambonie G; Groupe Francophone de Réanimation et d’Urgences Pédiatriques (GFRUP). High flow nasal cannula (HFNC) versus nasal continuous positive airway pressure (nCPAP) for the initial respiratory management of acute viral bronchiolitis in young infants: a multicenter randomized controlled trial (TRAMONTANE study). Intensive Care Med. 2017 Feb;43(2):209-216. doi: 10.1007/s00134-016-4617-8. Epub 2017 Jan 26. PMID: 28124736
27. Hutchings FA, Hilliard TN, Davis PJ. Heated humidified high-flow nasal cannula therapy in children. Arch Dis Child. 2015 Jun;100(6):571-5. doi: 10.1136/archdischild-2014-306590. Epub 2014 Dec 1. PMID: 25452315
28. Fuchs H, Klotz D, Nicolai T. Nichtinvasive Beatmung bei Kindern mit akuter respiratorischer Insuffizienz [Noninvasive ventilation in pediatric acute respiratory failure]. Notf Rett Med. 2017;20(8):641-648. German. doi: 10.1007/s10049-017-0368-5. Epub 2017 Oct 2. PMID: 32288636; PMCID: PMC7101806
29. Alansari K, Toaimah FH, Almatar DH, El Tatawy LA, Davidson BL, Qusad MIM. Monoclonal Antibody Treatment of RSV Bronchiolitis in Young Infants: A Randomized Trial. Pediatrics. 2019 Mar;143(3):e20182308. doi: 10.1542/peds.2018-2308. Epub 2019 Feb 13. PMID: 30760509
30. Hanna S, Tibby SM, Durward A, Murdoch IA. Incidence of hyponatraemia and hyponatraemic seizures in severe respiratory syncytial virus bronchiolitis. Acta Paediatr. 2003 Apr;92(4):430-4. doi: 10.1111/j.1651-2227.2003.tb00573.x. PMID: 12801108
31. Friedman JN, Rieder MJ, Walton JM; Canadian Paediatric Society, Acute Care Committee, Drug Therapy and Hazardous Substances Committee. Bronchiolitis: Recommendations for diagnosis, monitoring and management of children one to 24 months of age. Paediatr Child Health. 2014 Nov;19(9):485-98. doi: 10.1093/pch/19.9.485. PMID: 25414585; PMCID: PMC4235450.
32. National Institute for Health and Care Excellence. Bronchiolitis: diagnosis and management of bronchiolitis in children. Clinical Guideline NG 9. June 2015. https://www.nice.org.uk/guidance/ng9 (Accessed on August 20, 2015).








Add comment