25 November 2024, by Shahriar Lahouti.
Introduction
Diabetic ketoacidosis (DKA) is an acute, life-threatening complication of diabetes mellitus and usually presents with acidotic pH. However, the mixed acid-base disorder is not rare, and diabetic ketoacidosis presenting with alkalosis (aka. “ketoalkalosis”, “masked DKA” or “alkaline ketoacidosis”) have been reported in several case series *,*,*,*.
Case Presentation
A 27-year-old male with a history of type 1 DM presents to the emergency department with complaints of intractable vomiting, generalized weakness, and abdominal pain for the last 10 hours. He was diagnosed with type 1 DM about 10 years ago with the last hemoglobin A1C of 9.5 (3 weeks before admission). He was prescribed insulin Lantus 30 units once a day along with insulin aspart 8 units along with three meals. The patient noticed non-adherence to insulin dosages during the current illness and states that diabetes and vomiting have been a real problem because of frequent admissions to the hospital.
- Initial vital signs: Afebrile, blood pressure 97/54 mm Hg, respiratory rate 26/min, pulse 115/min, oxygen saturation 99% in room air, body mass index (BMI) 23.2.
- ECG: Normal sinus rhythm with a rate of 110/min.
- On admission, he was lethargic, with rapid and deep breathing (kussmaul respiration), and severe epigastric abdominal pain.
- Point-of-care ultrasound: Small IVC with >50% collapsibility and hyperkinetic heart.
- Initial lab investigations revealed: blood glucose 418 mg/dL, serum sodium 138 meq/dL, chloride 94 meq/L, potassium 3.5 meq/L, and moderate amounts of urinary ketones. The corrected anion gap was 24.3 meq/L. AG Calculator 🧮
- Arterial blood gas analysis showed pH 7.56, PCO2 27 mm Hg, and bicarbonate 21 mmol/L. Other labs are mentioned in the table below.
| Biochemical profile | On admission | After IV fluid resuscitation |
| Arterial blood gas pH | 7.56 | 7.24 |
| PCO2 (mm Hg) | 27 | 33 |
| Bicarbonate (mmol/L) | 21 | 14 |
| Sodium (meq/L) | 138 | 133 |
| Potassium (meq/L) | 3.5 | 3.4 |
| Chloride (meq/L) | 94 | 100 |
| Albumin (G/L) | 3.2 | 3.5 |
| Glucose (mg/dL) | 418 | 285 |
| Blood urea nitrogen (mg/dL) | 24 | 24 |
| Creatinine (mg/dL) | 0.7 | 0.6 |
| Lactic acid | 2.1 | 1.7 |
| Urinary ketones | Moderate | – |
| Corrected anion gap | 24.3 | 20.5 |
| Delta-delta ratio | ~4 | 0.85 |
Moderate amounts of urine ketones and a high anion gap in the context of hyperglycemia suggest diabetic ketoacidosis. however, a pH of 7.56 does not fulfill the diagnostic triad of DKA. In this case, a delta-delta ratio of four unmasks the presence of mixed acid-base disorder 👉”high anion gap metabolic acidosis” plus “metabolic alkalosis” (discussed below).
Treatment with intravenous (IV) saline, potassium replenishment, and IV insulin was started immediately. After receiving 3 liters of IV saline, the patient was awake and alert. Repeating the metabolic panel revealed the above values after initial fluid resuscitation.
Discussion
🔳Background
- Diabetic ketoacidosis (DKA) is due to absolute or relative insulin deficiency (more on the pathophysiology of DKA, see here).
- The diagnosis of DKA is based on the triad of hyperglycemia, ketosis, and metabolic acidosis.
- Although different professional societies have agreement on the main diagnostic feature of DKA which is the elevation in circulating total blood ketone level, the other diagnostic criteria, such as serum glucose and bicarbonate levels, differ *.
- “Pure” DKA is defined as pH ≤ 7.3, bicarbonate ≤15, and an anion gap (AG) >12 with positive serum and/or urine ketones. Blood glucose is usually ≥250 mg/dL but can be lower, especially with the use of SGLT2 inhibitors *.
- Diagnosis is more challenging in the presence of mixed acid-base disorders (e.g. associated vomiting, which will raise the bicarbonate level) *.
🔳Ketoalkalosis (aka. “masked DKA” or “alkaline ketoacidosis”)
- Refers to cases of ketoacidosis in which the acidosis is masquerade by a coexisting alkalosis. The term ‘diabetic ketoalkalosis’ first appeared in a case report in
1970 *. - Causes of alkalemia in DKA patients:
- Recurrent vomiting
- This will cause metabolic alkalosis due to hydrogen ion loss from the gastrointestinal tract and contraction alkalosis due to volume depletion.
- Patients with DKA commonly present with profuse vomiting. There is also evidence that patients having autonomic neuropathy such as gastroparesis due to poorly controlled diabetes, usually present with recurrent vomiting *.
- Alkali ingestion.
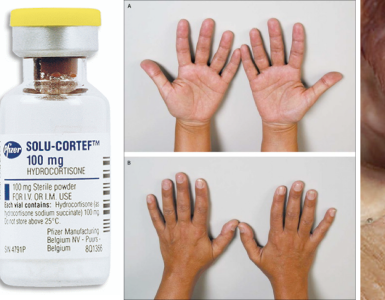
- Hypercortisolism *
- Contraction alkalosis due to dehydration and/or diuretic use.
- Recurrent vomiting
🔳Clinical presentation
- Clinical presentation of DKA includes symptoms and signs of:
- Hyperglycemia: Polyuria, polydipsia, weakness, signs of circulatory volume depletion such as tachycardia, decreased skin turgor, and capillary refill *.
- Acidosis: Nausea, vomiting, abdominal pain, altered sensorium, air hunger, and kussmaul respiration.
- Precipitating illness (e.g. infection, myocardial infarction, stroke).
🔳Diagnostic evaluation
- Lab investigations for diagnosis of DKA include:
- Blood glucose.
- Note that blood glucose could be normal in euglycemic DKA.
- Serum and/or urinary ketone
- Chemistry panel
- Calculating the anion gap and delta-delta ratio helps to reveal the mixed acid-base disorders *.
- Blood glucose.
- Evaluate for other causes of elevated anion gap e.g. lactic acidosis by sepsis, salicylate overdose, uremia, or toxic alcohol ingestion *.
- Evaluate for the precipitating causes of DKA (if it is unclear):
- Complete blood count with a differential, ECG, urinalysis, +/- urine & blood culture.
🔳Is blood gas analysis helpful in the diagnosis of DKA?
- Although current guidelines widely recommend obtaining blood gases, neither VBG nor ABG is usually helpful in diagnosing DKA.
- Blood gas provides information only regarding the respiratory component of pH (i.e. PCO2).
- If the chemistry panel is evaluated and a comprehensive history and physicals are performed, blood gas analysis (i.e. pH, PCO2) usually will not have a major effect on the diagnosis and management of the patients *.
- The diagnosis of diabetic ketoacidosis should be based on an analysis of the metabolic derangements in the acid-base status (e.g. anion gap, beta-hydroxybutyrate level).
- As explored above, pH could be normal or even alkalotic in patients with underlying DKA.
🔳Diagnosis of masked DKA (aka. “ketoalkalosis”, or “alkaline ketoacidosis”)
- Diagnosis of DKA should be suspected whenever patients have significant hyperglycemia, especially if they are ill or highly symptomatic.
- Suspecting DKA, the clinician should calculate for the mixed acid-base disorder by calculating the anion gap and the delta–delta ratio.
- Patients with masked DKA often present with hyperglycemia >250 mg/dL, normal or alkalotic pH, and bicarbonate >20 meq/L (which does not meet the criteria for DKA).
- An elevated AG in this context is suggestive of ketoacidosis (however other causes of high AG need to be eliminated e.g. lactate, toxic alcohols, salicylates).
- A delta–delta ratio > ~1.6 will support the presence of metabolic alkalosis *.
- Following the administration of IV fluid and replacement of electrolytes, diagnosis of DKA becomes evident on laboratory analysis.
🔳Treatment of diabetic ketoalkalosis
- Treatment of diabetic ketoalkalosis does not differ from the conventional management of DKA (discussed here). These patients should be treated with
- Aggressive IV fluids
- Electrolyte supplementation (especially potassium)
- Insulin IV infusion.
⭐️Administration of IV fluids with timely replenishment of electrolytes remains of utmost priority.
Learning Points
- The absence of low serum bicarbonate or low pH does not rule out DKA, as there may be a mixed acid-base disorder.
- Calculating the anion gap and the delta–delta ratio will detect the underlying mixed acid-base disorder.
- Treatment of diabetic ketoalkalosis follows the conventional treatment of DKA with IV fluid, insulin infusion, and electrolyte replacement (especially potassium).
Going further
- DKA: Mind the gap!
- Resuscitation of Adult Diabetic Ketoacidosis
- Acid-Base Disorders in Critically Ill Patients: A Systematic Approach
References
1. KUMAR, V., NANAVATI, S., KOMAL, F., ORTIZ, L., PAUL, N., KUMAR, M., MICHAEL, P., SINGHAL, M.. Ketoalkalosis: Masked Presentation of Diabetic Ketoacidosis With Literature Review. Journal of Endocrinology and Metabolism, North America, 7, Jan. 2018.
2. PMID: 30279254. Nanavati S, Kumar V, Melki G, Singhal M. Diabetic ketoalkalosis: misnomer or undiagnosed variant of diabetic ketoacidosis. BMJ Case Rep. 2018 Oct 2;2018:bcr2018226092. doi: 10.1136/bcr-2018-226092.
3. PMID: 19117632. Watanabe Y, Noda K, Akazawa K, Fukuyama J. Two cases of type 1 diabetic women with diabetic ketoacidosis presenting as alkalemia. Diabetes Res Clin Pract. 2009 Feb;83(2):e54-7. doi: 10.1016/j.diabres.2008.11.020. Epub 2008 Dec 30.
3. PMID: 25653472. Svart MV, Voss TS, Bayat M, Madsen LR, Andersen LT, Poulsen PL, Møller N. Rare presentations of ketoacidosis: diabetic ketoalkalosis and ketoacidosis secondary to fasting and muscular dystrophy. Clin Diabetes. 2015 Jan;33(1):37-9. doi: 10.2337/diaclin.33.1.37.
4. PMID: 29650082. Diabetes Canada Clinical Practice Guidelines Expert Committee; Goguen J, Gilbert J. Hyperglycemic Emergencies in Adults. Can J Diabetes. 2018 Apr;42 Suppl 1:S109-S114. doi: 10.1016/j.jcjd.2017.10.013.
5. PMID: 4982832. Roggin GM, Moses D, Kautcher M, Wishner W, Shuman C. Ketosis and metabolic alkalosis in a patient with diabetes. JAMA. 1970 Jan 12;211(2):296-8.
6. PMID: 25651248. Kamel KS, Halperin ML. Acid-base problems in diabetic ketoacidosis. N Engl J Med. 2015 Feb 5;372(6):546-54. doi: 10.1056/NEJMra1207788.
7. PMID: 8968687. Elisaf MS, Tsatsoulis AA, Katopodis KP, Siamopoulos KC. Acid-base and electrolyte disturbances in patients with diabetic ketoacidosis. Diabetes Res Clin Pract. 1996 Sep;34(1):23-7. doi: 10.1016/s0168-8227(96)01332-0




Add comment