July 11, 2024, by Shahriar Lahouti. Last Update 15 September 2025.
CONTENTS
- Preface
- Pathophysiology
- Agents
- Approach to diagnosis and treatment
- Management
- Tricyclic antidepressant toxicity- Rapid review
- References
Preface
Voltage-gated sodium channels are present in many tissue types within the human body, including cardiac and neuronal tissues. Medications that act by sodium channel blockade have different clinical applications. Sodium channel blocker toxicity, whether intentional or accidental, can lead to catastrophic effects, including death. Understanding the effective treatment of toxicity caused by these medications is crucial, especially in patients with critical poisoning.
Pathophysiology
▪️Defining sodium channel blockers
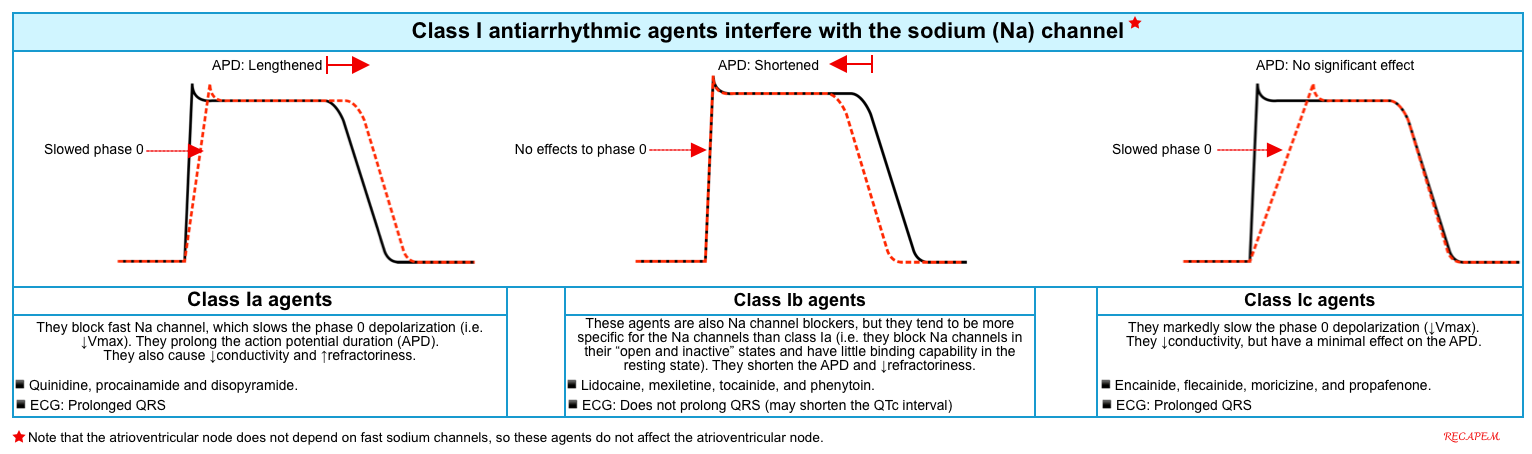
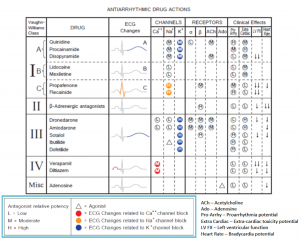
- Sodium-channel blocker is used here to refer to those agents that block cardiac fast sodium channels with properties similar to class Ia or Ic antidysrhythmics *.
- Antiarrhythmic class Ia or Ic causes a slowing of phase zero depolarization in cardiomyocytes (figure below) *.
- Slowing phase-zero depolarization results in QRS prolongation.
- Note that the “sodium-channel blocker” in this context does not include class Ib antiarrhythmics (e.g., lidocaine), even though lidocaine does inhibit sodium channels.
- Lidocaine doesn’t affect phase-zero depolarization, nor does it prolong the QRS complex *.
- Lidocaine can reduce the action potential duration, making it useful in the treatment of arrhythmias caused by class Ia or class Ic intoxication (this will be discussed below). Lidocaine’s ability to shorten the QTc interval makes it useful in the management of torsade de pointes *.
- Antiarrhythmic class Ia or Ic causes a slowing of phase zero depolarization in cardiomyocytes (figure below) *.
Agents
- Antidysrhythmics *
- Tricyclic antidepressants
- Amitriptyline, desipramine, clomipramine, nortriptyline, imipramine, maprotiline.
- Local anesthetics
- Amide local anesthetics: Bupivacaine, lidocaine, ropivacaine.
- Ester local anesthetics: Cocaine, procaine.
- Other antidepressants
- SSRI: Citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine.
- SNRI: Venlafaxine
- DNRIs (dopamine-norepinephrine uptake inhibitors): bupropion.
- Antihistamines
- Dimenhydrinate, diphenhydramine, orphenadrine, chlorpheniramine, terfenadine.
- Antipsychotics
- Chlorpromazine, fluphenazine, thioridazine, and loxapine.
- Antiepileptics
- Carbamazepine, lamotrigine, lacosamide, zonisamide, and topiramate.
- Opioids
- Buprenorphine, methadone, propoxyphene, tramadol.
- Muscle relaxants
- Orphenadrine, cyclobenzaprine *.
- Antimalarials
- Chloroquine, hydroxychloroquine, quinine.
- Miscellaneous
Approach To Diagnosis and Treatment
Although the list of agents causing cardiocyte sodium-channel blockade is broad and the clinical features are variable, the initial treatment plan is almost the same. The initial treatment for toxicity due to sodium channel blockers should not be delayed until definitive drug test results become available.
The mnemonic SALT describes the signs and symptoms of sodium channel blockade toxicity: Shock, Altered mental status, Long QRS, and Terminal R in aVR *.
The diagnostic and therapeutic approach to patients with sodium-channel blocker intoxication follows the same principles as the general approach to drug poisoning in adults. However, several helpful points should be mentioned here.
Clinical features
⚠️CAUTION: Patients with sodium channel blocker intoxication may be initially asymptomatic but may deteriorate rapidly.
▪️Cardiovascular system *
- Dysrhythmias
- Hypotension
- Cardiovascular collapse.
▪️CNS
- Altered mental status, agitation, delirium, sedation, and coma.
- Seizures *.
▪️Other features
- Sodium channel blockers also affect other cardiac receptors and ion channels * (figure below).
- Many of the sodium channel blockers have anticholinergic effects, and patients may present with simultaneous anticholinergic toxidrome, e.g., delirium, dry and flushed skin, pupillary dilation, and urinary retention.
Evaluation
History & Physical Exam
▪️History
- Medication list
- Consider the potential use of other substances (e.g., ethanol, cocaine, opioids), and co-ingestion of over-the-counter medications (e.g., acetaminophen, aspirin).
- Timing (the last time the patient was known to be well) & amount of ingestions.
▪️Physical exam
- Specific exam findings may identify a toxidrome, such as anticholinergic, and help determine the extent of toxicity or identify potential drugs involved in the overdose. This includes evaluation for:
- Vitals: Temp, blood pressure, heart rate, and respiratory rate?
- Mental status
- Pupillary size
- Skin: Extremely diaphoretic or dry, skin flushing
- Muscle rigidity
- Tremor
- Ankle clonus.
Initial investigation
- Fingerstick glucose (for anyone with an altered mental status).
- ECG
- Blood count, electrolyte, renal, and hepatic profiles, arterial or venous blood gas.
- Acetaminophen and salicylate levels, to rule out these common co-ingestants.
ECG Findings
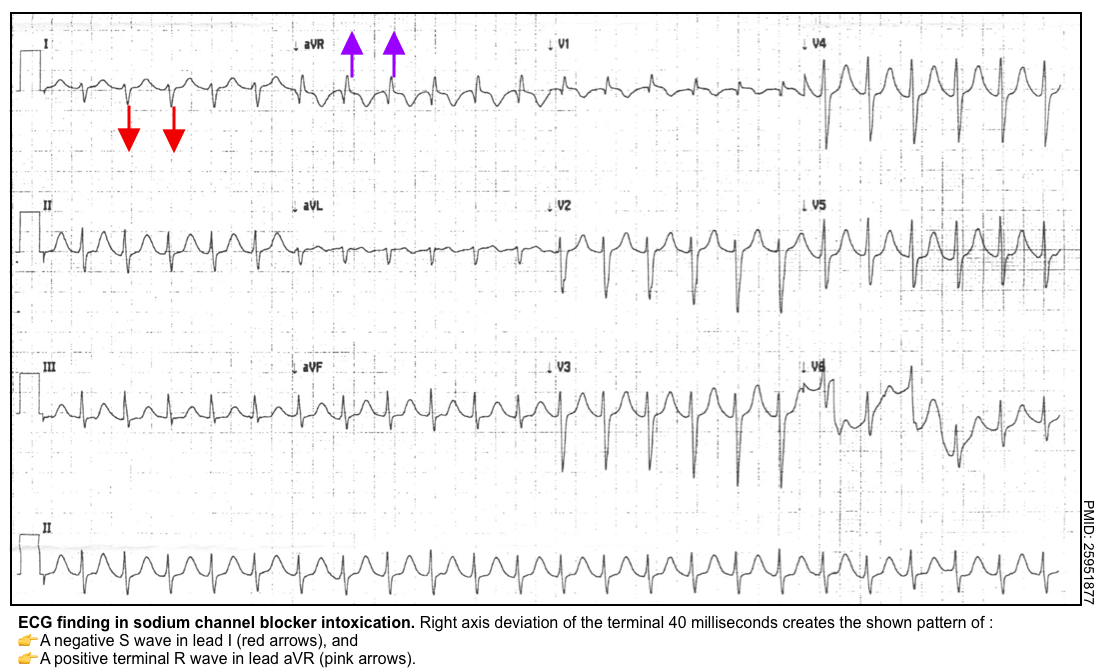
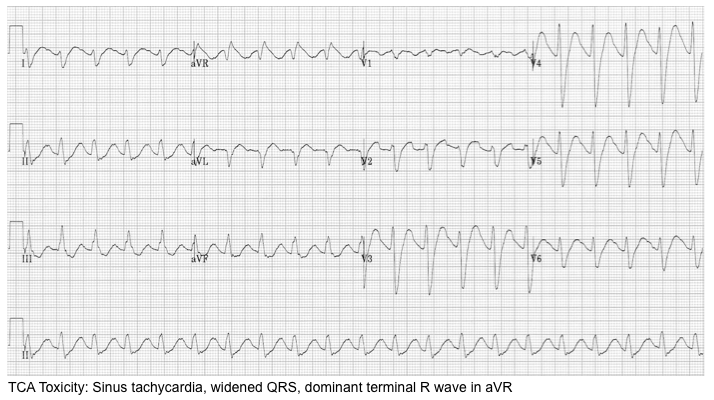
Terminal right axis deviation
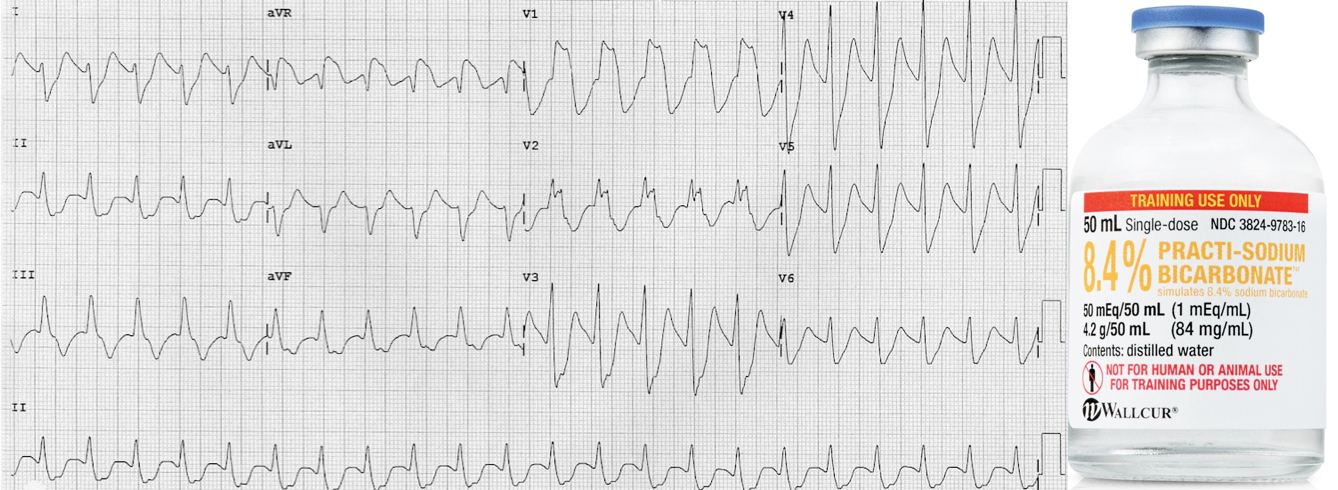
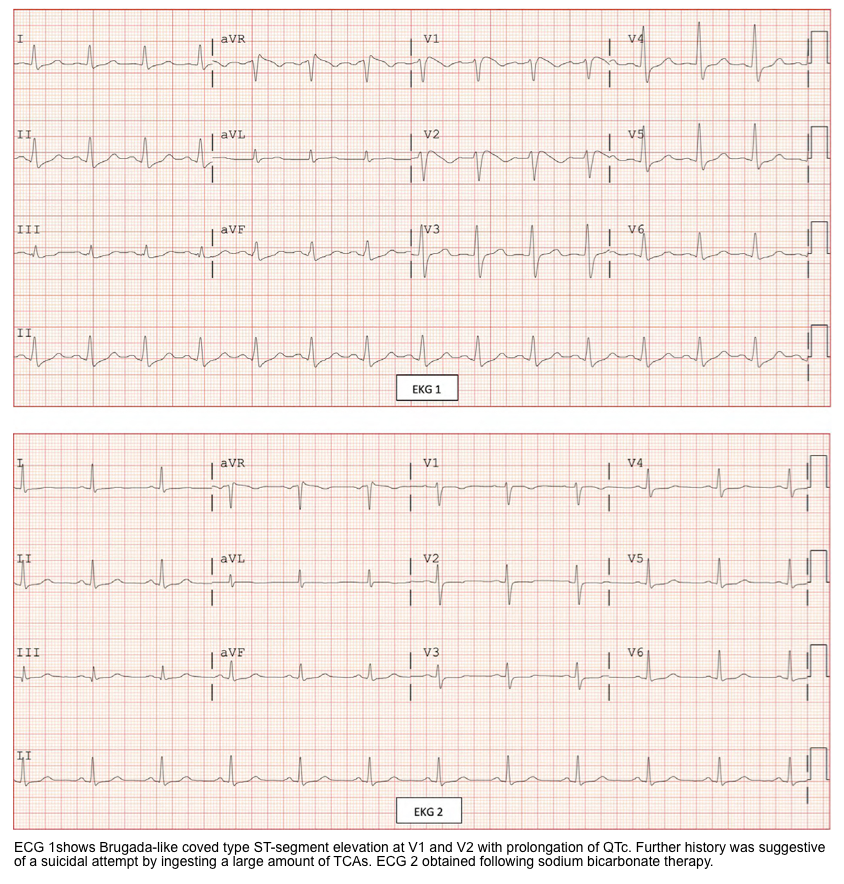
▪️Electrophysiologically, this is caused by slow conduction through the myocardium, leading to delayed depolarization of the right ventricle (such that the terminal 40 msec of the QRS complex points in a rightward direction). This creates the following pattern (ECG below):
- Deep, terminal S-wave in Lead I (which may be broad or slurred).
- Terminal tall R-wave in aVR.
▪️Diagnostic consideration
- This classic ECG pattern is seen frequently in moderate to severe cyclic antidepressant toxicity, but its absence does not eliminate the possibility of toxicity, and life-threatening complications can occur in the absence of significant ECG abnormalities *.
- A tall R-wave in aVR (R-wave >3 mm or an R/S ratio >0.7) predicts a risk of developing seizure or arrhythmia among patients with TCA intoxication *,*.
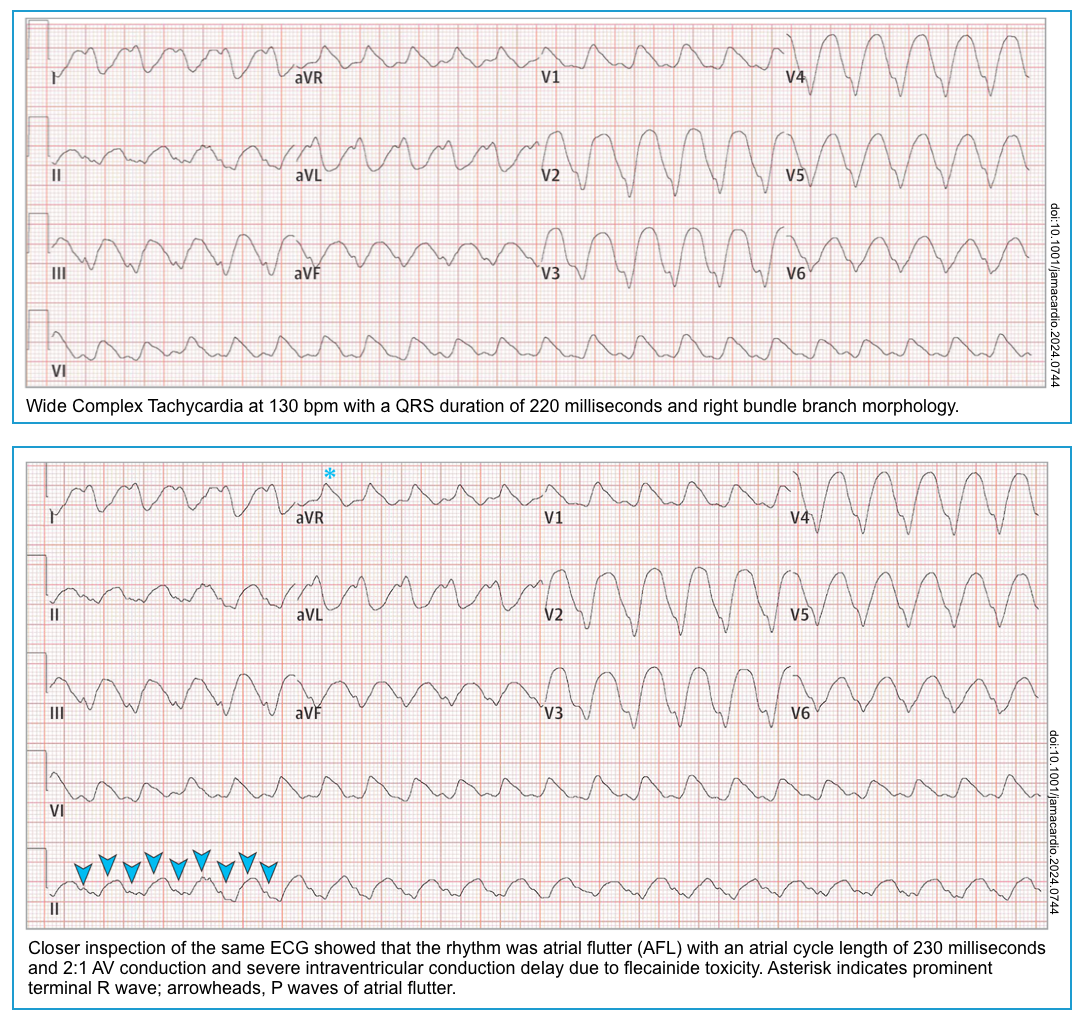
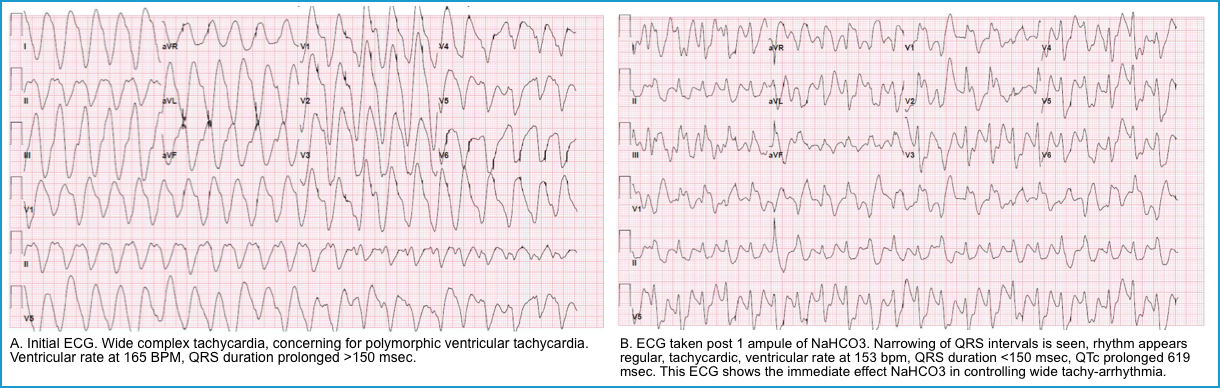
QRS Widening
▪️Widening of the QRS complex is not specific for sodium channel blockers; however, in patients with normal baseline ECG and QRS widening following TCA intoxication, the QRS duration has prognostic and therapeutic significance:
- QRS >100 ms suggests an elevated risk of seizures *.
- A new (or presumably new) QRS >100 ms is an indication for the administration of sodium bicarbonate *.
- QRS >160 ms suggests an elevated risk of ventricular tachycardia *.
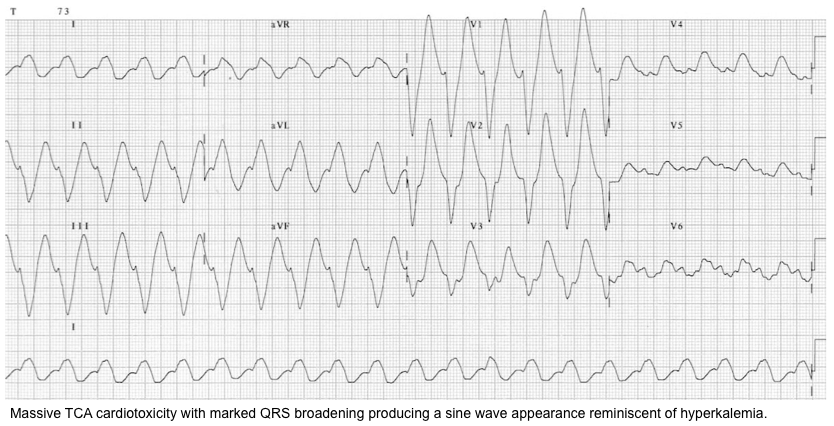
⭐️In severe intoxication, the QRS complex may become profoundly broad, producing a sine wave pattern.
- Sinus tachycardia with a wide QRS interval may mimic ventricular tachycardia (ECG below).
- 👉The differential diagnosis of wide-complex tachycardia is discussed here.
Brugada pattern type I
The Brugada type I pattern reflects sodium channel insufficiency due to acquired causes and/or a genetic channelopathy. This can occur in different contexts:
- Patients with genetic abnormalities and Brugada syndrome may have this abnormality on their baseline ECG.
- Patients with subtle alterations of their sodium channels may manifest this ECG pattern only after a variety of physiologic stressors (e.g., fever, hypothermia, hyperkalemia *).
- Patients with normal sodium channels may manifest this abnormality due to an overdose of sodium channel-blocking agents *.
- This can be seen in roughly 10-15% of patients with TCA poisoning who require ICU admission, but is rarely seen in other overdoses *.
Overall, the Brugada type I pattern is not diagnostic of sodium channel blocker overdose. However, the pattern should be recognized since it can support this diagnosis within the appropriate context *.
The Brugada type I pattern is marked by the following findings in V1, V2, or multiple leads within V1-V3:
- Coved ST elevation followed by a T-wave inversion.
- No well-defined r’ wave.
- Gentle downslope from the QRS complex into the T-wave (this is more gradual than with the right bundle branch block).
Other findings
- RBBB (right bundle branch block)
- QT interval prolongation is secondary to slow ventricular depolarization.
- However, torsade de pointes doesn’t commonly occur (since most patients with TCA overdose are commonly tachycardic).
- Sinus tachycardia is protective against severe QT interval prolongation and afterpotential generation.
- However, torsade de pointes doesn’t commonly occur (since most patients with TCA overdose are commonly tachycardic).
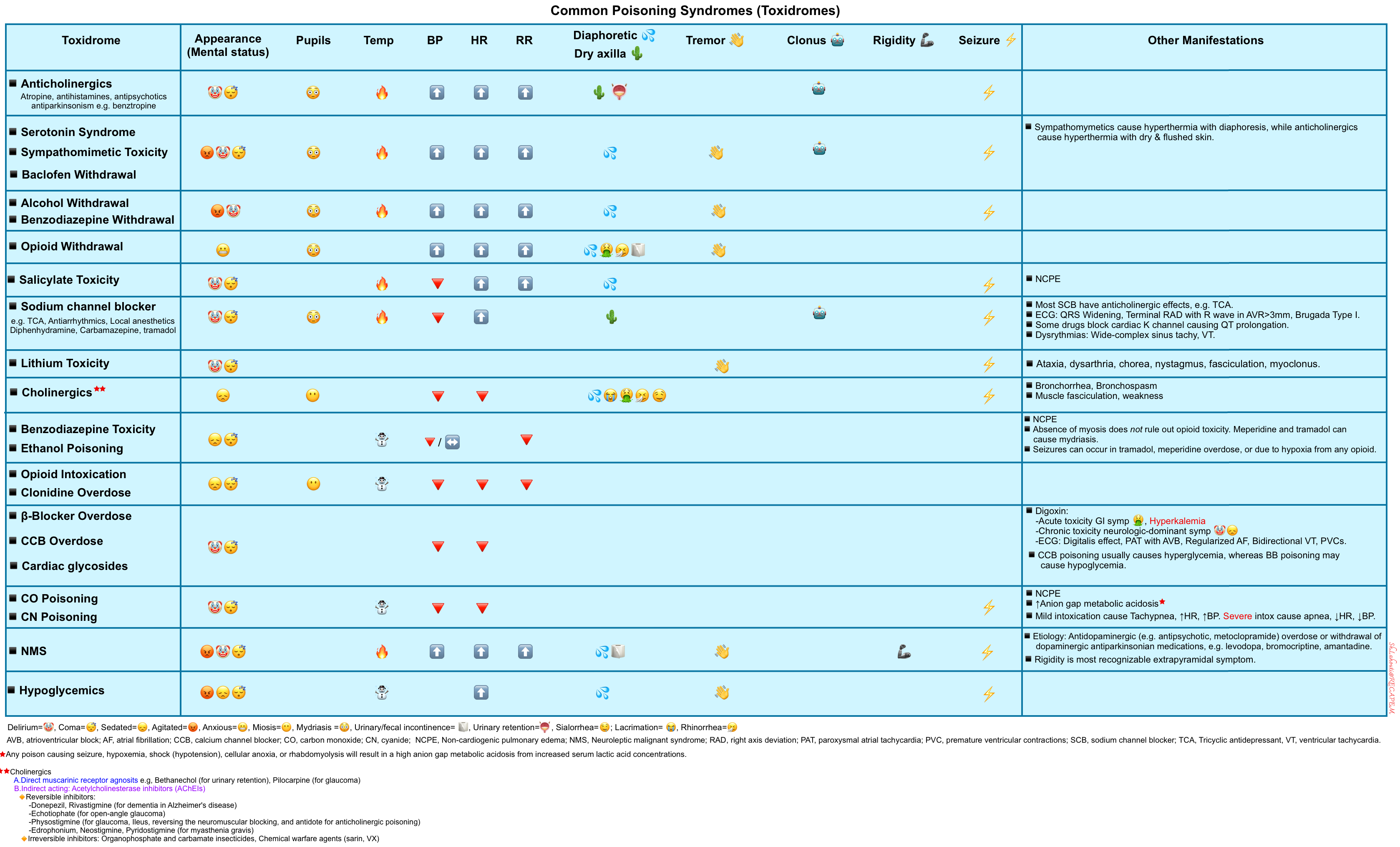
Differential diagnosis
The differential diagnosis of patients presenting with sodium channel blocker toxicity is broad, given the range of clinical findings (decreased level of consciousness, seizures, anticholinergic effects, hypotension, widening of the QRS interval, etc.) associated with this poisoning. In addition to sodium channel blockers, including TCA
toxicity, these findings are associated with several other poisonings (toxidromes, table below).
- QRS widening may be due to sodium channel blockers (discussed above) or preexisting conduction delay.
- For common causes of toxicologic seizure, see 👉here.
- Toxicologic causes of delirium are discussed here.
Management
Principles
▪️The general approach to the management of intoxicated patients is discussed separately.
▪️Sodium channel blocker toxicity can cause critical poisoning, defined as those in cardiac arrest, refractory shock, or other conditions posing an imminent threat of cardiac arrest *. Treatment and stabilization of these patients must be performed before the involved poison is known.
- Intubation
- The indications for intubation in patients with unknown poisoning are discussed separately.
- In patients with sodium channel blocker toxicity, consider intubation for:
- Decreased or deteriorating level of consciousness
- Seizures, including status epilepticus.
- Hypoventilation with respiratory acidosis (this will worsen sodium channel blocker intoxication) *.
- Support hemodynamics with a vasopressor before proceeding to intubation.
- Consider apneic ventilation via a BiPAP machine or ventilator (to minimize the acidosis, as it worsens the toxicity associated with Na+ channel blockers).
- Consider a mild hyperventilation (e.g., Target end-tidal CO2 20-25 mmHg) as alkalemia has therapeutic implications in this context.
- Hypotension
- The general management strategy is discussed in detail here.
- Hypotension should be treated initially with isotonic crystalloid fluids; however, most intoxicated patients are not hypovolemic.
- Start bicarbonate for hypotension that isn’t due to hypovolemia.
- Vasopressor initiation should not be delayed while waiting to see if volume will work.
- Vasopressors should be used when hypotension is unresponsive to fluids and sodium bicarbonate therapy:
- Epinephrine may be a favorable choice for patients with bradycardia.
- Norepinephrine is preferred if the heart rate is normal or mildly elevated. For markedly tachycardic patients, phenylephrine may be a better choice.
- Vasopressin can be tried if there is no response to norepinephrine or epinephrine *.
- Mechanical support of the circulation with cardiopulmonary bypass, overdrive pacing, or aortic balloon pump assistance may be warranted in patients with refractory hypotension.
- The general management strategy is discussed in detail here.
▪️Treatment of cardiac arrest and life-threatening toxicity often requires specialized treatments that are not commonly employed (e.g., antidotes), in addition to effective basic and advanced life support *. In the following discussion, specific therapeutic measures for patients with sodium channel blocker toxicity are explored.
Treatment
Treatment recommendations for poisoning by other sodium channel blockers are often extrapolated from TCA studies.
- No studies have compared treatments during cardiac arrest from sodium channel blocker poisoning *.
- Human evidence is limited to retrospective observational studies and case reports, in which patients received multiple interventions. The vast majority of these involve TCA poisoning. The therapeutic intervention with the most evidence is hypertonic sodium bicarbonate administration and induction of alkalemia, which are variably beneficial in case reports and animal models *.
Sodium Bicarbonate
▪️Mechanism of action
- Sodium bicarbonate alters the interaction between the xenobiotic and cardiac sodium channels via the following two mechanisms:
- Sodium-dependent effect
- Hypertonic sodium bicarbonate increases the availability of Na ions to pass through the open channels.
- Sodium displaces Na channel-blocking drugs from the channel itself.
- pH-dependent effect
- Both the ionized and the nonionized forms of xenobiotics can bind to the Na channel, but the ionized form accounts for 90% of the blockade.
- Bicarbonate increases the fraction of the nonionized xenobiotic and, therefore, limits the quantity of xenobiotics available to bind to the Na+ channel *.
- Sodium-dependent effect
- Sinus rhythm with QRS complex duration > 100 msec
- Hypotension refractory to IV fluid.
- Hypotension that does not improve with appropriate fluid challenges should be treated with sodium bicarbonate (regardless of QRS complex duration).
- Ventricular arrhythmia
- Seizure *
▪️Target 🎯 and therapeutic goals
- QRS < 100 msec.
- Elevated pH to 7.50-7.55
- Resolution of hypotension.
| ⚠️Avoid complications of bicarbonate therapy including * ▪️Hypernatremia (serum sodium not to exceed 150–155 mEq/L) ▪️Alkalemia (pH>7.55) ▪️Hypokalemia ▪️Hypocalcemia |
▪️Monitoring during treatment
- Continuous 12-lead ECG monitoring *
- Arterial pH measurement
- It should be measured hourly until it falls within the therapeutic range and is stable. After that, measurements may be obtained every four to six hours.
- Serum potassium
▪️Administration
- Initial bolus doses
- Hypertonic sodium bicarbonate
- 1-2 mEq/kg (~2 vials of prefilled syringes, each 50mL of 8.4% NaHCO3) given as a rapid IV push through a large-bore IV catheter.
- It may be repeated every 5 minutes as needed to decrease the QRS interval.
- If the QRS interval doesn’t change despite 100-200 mEq (2-4 ampules), this raises the question of whether the diagnosis may be incorrect.
- However, severe cases may occasionally require massive doses of hypertonic bicarbonate (e.g., 10-30 ampules) *.
- Hypertonic sodium bicarbonate
- Maintenance dose
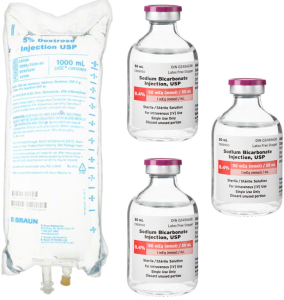
- Isotonic bicarbonate
- This can be prepared by mixing 150 mEq of sodium bicarbonate in 1 L of D5W (figure below).
- Infusion rate: 150-250 mL/hour in adults.
- Note that isotonic bicarbonate is less effective than hypertonic bicarbonate because it lacks the effect of hypertonic sodium on the cardiac sodium channels. Nonetheless, maintaining an alkalemic pH may be beneficial in TCA intoxication to reduce the free drug level.
- Isotonic bicarbonate
- Weaning off
- Bicarbonate therapy can be tapered off after the resolution of ECG changes, which may occur over hours to days.
- It is reasonable to reduce the infusion rate by about 25% per hour over 4 hours.
- If the QRS interval widens during tapering, give an additional bolus of sodium bicarbonate as above and restart the original infusion rate.
- Bicarbonate therapy can be tapered off after the resolution of ECG changes, which may occur over hours to days.
▪️Alternative to hypertonic bicarbonate treatment
- If necessary, serum sodium can be increased separately by administration of hypertonic saline *, and pH can be controlled by adjusting minute ventilation in intubated patients *.
| ▪️Hyperventilation is a reasonable alternative to sodium bicarbonate therapy in the setting of renal failure, pulmonary edema, or cerebral edema. Although hyperventilation is less effective in reversing toxicity *. ▪️Hypertonic saline 3% given as 1-3 mL/kg IV over 10 minutes, to decrease ventricular ectopy or dysrhythmia in a patient with cardiotoxicity refractory to sodium bicarbonate therapy *. |
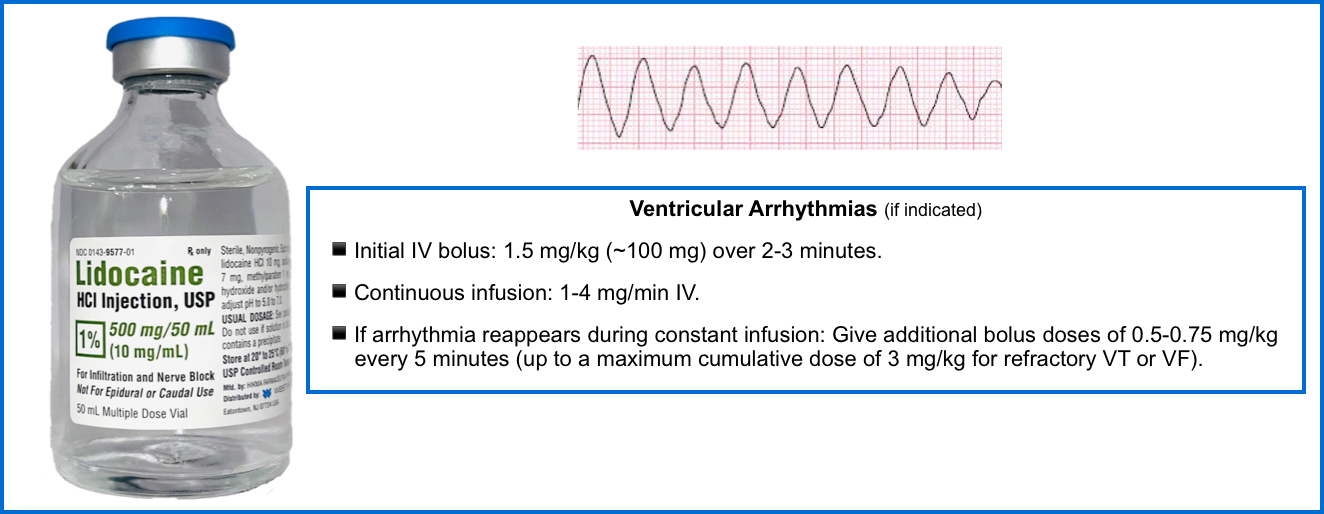
Lidocaine
- Recurrent ventricular arrhythmias (VT, VF) despite bicarbonate.
⚠️Lidocaine should be administered cautiously in patients with seizures *.
▪️Mechanism of action
- Lidocaine competes with class Ia and Ic antidysrhythmics for binding at the sodium channel and dissociates from the receptor more rapidly than class Ia or Ic agents
such as TCAs and therefore does not depress phase 0 depolarization *. - Lidocaine theoretically may be more effective against agents that bind to sodium channels for prolonged periods of time (e.g., amitriptyline and nortriptyline), as opposed to agents that bind to sodium channels for shorter periods of time (e.g., imipramine or desipramine) *.
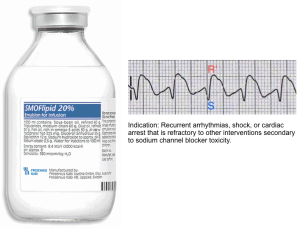
Intravenous lipid emulsion (ILE)
▪️Indication
- Life-threatening sodium channel blocker poisoning ( arrhythmias, shock, or cardiac arrest ) refractory to other treatment modalities *.
▪️Mechanism of action
- IV lipid emulsion creates a “lipid sink” that sequesters the drug and prevents toxicity *.
▪️Dosing
- The recommended dosing schema for 20% lipid emulsion is based on that recommended for local anesthetic systemic toxicity *:
- Give a bolus of 1.5 ml/kg over ~2-3 minutes (e.g., ~100 ml). Repeat bolus may be considered if no response to the first bolus.
- Following the initial bolus, an infusion is started at a rate of 0.025 mL/kg per minute (1.5 mL/kg/hour) until hemodynamic recovery occurs.
- If hemodynamic instability persists, the drip may be continued for one hour, with a maximum dose of 8 mL/kg over that hour and 12.5 mL/kg in 24 hours.
Management of seizures
▪️Background
- The incidence of seizures is similar to ventricular tachycardia and occurs in an estimated 4% of patients presenting with overdose.
- Most seizures are typically generalized and of brief duration *.
- Focal seizures and status epilepticus are atypical and should prompt further neurologic evaluation.
- Multiple seizures occur in ~10% to 30% of cases of cyclic antidepressant overdose.
- Seizures are extremely dangerous in the context of TCA intoxication.
- These may cause acidosis, which increases free tricyclic levels and leads to a death spiral.
- Abrupt deterioration in hemodynamic status, namely hypotension and ventricular dysrhythmias, often develops during or within minutes after a seizure. This rapid cardiovascular deterioration likely results from seizure-induced acidemia that exacerbates cardiovascular toxicity.
- In patients with TCA intoxication, seizures most often occur within 1 to 2 hours of ingestion.
▪️Immediate therapy
- Benzodiazepines are given to control the seizures *.
- Sodium bicarbonate should be started.
- Note that bicarbonate does not stop seizures, but it limits further acidosis (which increases the risk of arrhythmias) and the transit of TCA into the CNS *.
▪️Benzidiazepine-resistant seizures and status epilepticus
- Barbiturates (e.g., phenobarbital) are indicated to treat seizures resistant to benzodiazepines.
- However, they are considered second-line therapy due to their adverse effects on blood pressure.
- Intubation is indicated for ongoing seizures or a decreased level of consciousness.
- Following intubation, propofol or benzodiazepines should be used for the dual purpose of sedation and seizure management *.
⚠️Phenytoin should be avoided as it may worsen the sodium channel blockade *.
Management of ventricular tachycardia
- Wide complex tachycardia is discussed separately. More on the differential diagnosis of wide complex tachycardia here.
- Ventricular tachycardia in unstable patients should be cardioverted electrically. If cardioversion is not successful, the following medications should be given, and electrical cardioversion should be repeated.
-
- Note that sodium bicarbonate should be given even if cardioversion was successful to prevent recurrence.
-
-
- Hypertonic bicarbonate
- Lidocaine
- ⚠️Avoid amiodarone and other antiarrhythmic agent in this context as these may further prolong the QTc.
- Magnesium may be successful for bicarbonate-resistant arrhythmias (e.g. 2 grams IV) *.
- Lipid emulsion
Tricyclic antidepressant toxicity- Rapid review👉 here
References
1. PMID: 38108133. Perman SM, et al. American Heart Association. 2023 American Heart Association Focused Update on Adult Advanced Cardiovascular Life Support: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2024 Jan 30;149(5):e254-e273. doi: 10.1161/CIR.0000000000001194. Epub 2023 Dec 18.
2. PMID: 30354657. Lei M, Wu L, Terrar DA, Huang CL. Modernized Classification of Cardiac Antiarrhythmic Drugs. Circulation. 2018 Oct 23;138(17):1879-1896. doi: 10.1161/CIRCULATIONAHA.118.035455. Erratum in: Circulation. 2019 Mar 26;139(13):e635. doi: 10.1161/CIR.0000000000000675
3. PMID: 1313200. Grant AO Jr. On the mechanism of action of antiarrhythmic agents. Am Heart J. 1992 Apr;123(4 Pt 2):1130-6. doi: 10.1016/0002-8703(92)91072-9.
4. Smith, S.W. (2016). Sodium Channel-Blocking Antidysrhythmics. In: Brent, J., Burkhart, K., Dargan, P., Hatten, B., Megarbane, B., Palmer, R. (eds) Critical Care Toxicology. Springer, Cham. https://doi.org/10.1007/978-3-319-20790-2_134-1
5. PMID: 28932601. Mirrakhimov AE, Ayach T, Barbaryan A, Talari G, Chadha R, Gray A. The Role of Sodium Bicarbonate in the Management of Some Toxic Ingestions. Int J Nephrol. 2017;2017:7831358. doi: 10.1155/2017/7831358. Epub 2017 Aug 8.
6. PMID: 18821491. Schwartz M, Patel M, Kazzi Z, Morgan B. Cardiotoxicity after massive amantadine overdose. J Med Toxicol. 2008 Sep;4(3):173-9. doi: 10.1007/BF03161197.
7. PMID: 18206559. Lester L, McLaughlin S. SALT: a case for the sodium channel blockade toxidrome and the mnemonic SALT. Ann Emerg Med. 2008 Feb;51(2):214. doi: 10.1016/j.annemergmed.2007.09.028.
8. PMID: 10452441. Harrigan RA, Brady WJ. ECG abnormalities in tricyclic antidepressant ingestion. Am J Emerg Med. 1999 Jul;17(4):387-93. doi: 10.1016/s0735-6757(99)90094-3.
9. PMID: 7618783. Liebelt EL, Francis PD, Woolf AD. ECG lead aVR versus QRS interval in predicting seizures and arrhythmias in acute tricyclic antidepressant toxicity. Ann Emerg Med. 1995 Aug;26(2):195-201. doi: 10.1016/s0196-0644(95)70151-6.
10. PMID: 19736278. Eyer F, Stenzel J, Schuster T, Felgenhauer N, Pfab R, von Bary C, Zilker T. Risk assessment of severe tricyclic antidepressant overdose. Hum Exp Toxicol. 2009 Aug;28(8):511-9. doi: 10.1177/0960327109106970. Epub 2009 Sep 7.
11. PMID: 4022081. Boehnert MT, Lovejoy FH Jr. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med. 1985 Aug 22;313(8):474-9. doi: 10.1056/NEJM198508223130804.
12. PMID: 21436332. Body R, Bartram T, Azam F, Mackway-Jones K. Guidelines in Emergency Medicine Network (GEMNet): a guideline for the management of tricyclic antidepressant overdose. Emerg Med J. 2011 Apr;28(4):347-68. doi: 10.1136/emj.2010.091553.
13. PMID: 30675825. Rivera-Juárez A, et al. Clinical Characteristics and Electrophysiological Mechanisms Underlying Brugada ECG in Patients With Severe Hyperkalemia. J Am Heart Assoc. 2019 Feb 5;8(3):e010115. doi: 10.1161/JAHA.118.010115.
14. PMID: 35371667. Jain A, Yagnik K, Hussain KM, Naik S, Sharma T, Shahab A, Khilan MH. Pyrexia Unmasking Brugada Syndrome: A Literature Review. Cureus. 2022 Feb 22;14(2):e22489. doi: 10.7759/cureus.22489.
15. PMID: 12015405. Goldgran-Toledano D, Sideris G, Kevorkian JP. Overdose of cyclic antidepressants and the Brugada syndrome. N Engl J Med. 2002 May 16;346(20):1591-2. doi: 10.1056/NEJM200205163462020.
16. PMID: 25373053. O’Sullivan JC, Johnson AD, Waterman MA. Comparative resuscitation measures for the treatment of desipramine overdose. Mil Med. 2014 Nov;179(11):1266-72. doi: 10.7205/MILMED-D-14-00050.
17. PMID: 28491675. Vu NM, Hill TE, Summers MR, Vranian MN, Faulx MD. Management of life-threatening flecainide overdose: A case report and review of the literature. HeartRhythm Case Rep. 2015 Dec 29;2(3):228-231. doi: 10.1016/j.hrcr.2015.12.013.
18. PMID: 15811881. Greene SL, Dargan PI, Jones AL. Acute poisoning: understanding 90% of cases in a nutshell. Postgrad Med J. 2005 Apr;81(954):204-16. doi: 10.1136/pgmj.2004.024794.
19. PMID: 26159649. Bruccoleri RE, Burns MM. A Literature Review of the Use of Sodium Bicarbonate for the Treatment of QRS Widening. J Med Toxicol. 2016 Mar;12(1):121-9. doi: 10.1007/s13181-015-0483-y.
20. PMID: 28228939. Amiri H, Zamani N, Hassanian-Moghaddam H, Shadnia S. Cardiotoxicity of tricyclic antidepressant treated by 2650 mEq sodium bicarbonate: A case report. JRSM Cardiovasc Dis. 2016 Dec 1;5:2048004016682178. doi: 10.1177/2048004016682178.
21. PMID: 11482860. Blackman K, Brown SG, Wilkes GJ. Plasma alkalinization for tricyclic antidepressant toxicity: a systematic review. Emerg Med (Fremantle). 2001 Jun;13(2):204-10. doi: 10.1046/j.1442-2026.2001.00213.x.
22. PMID: 12827118. McKinney PE, Rasmussen R. Reversal of severe tricyclic antidepressant-induced cardiotoxicity with intravenous hypertonic saline solution. Ann Emerg Med. 2003 Jul;42(1):20-4. doi: 10.1067/mem.2003.233.
23. PMID: 9737495. McCabe JL, Cobaugh DJ, Menegazzi JJ, Fata J. Experimental tricyclic antidepressant toxicity: a randomized, controlled comparison of hypertonic saline solution, sodium bicarbonate, and hyperventilation. Ann Emerg Med. 1998 Sep;32(3 Pt 1):329-33. doi: 10.1016/s0196-0644(98)70009-5.
24. PMID: 29669228. Goldstein JN, Dudzinski DM, Erickson TB, Linder G. Case 12-2018: A 30-Year-Old Woman with Cardiac Arrest. N Engl J Med. 2018 Apr 19;378(16):1538-1549. doi: 10.1056/NEJMcpc1800322.
25. PMID: 20507243. Foianini A, Joseph Wiegand T, Benowitz N. What is the role of lidocaine or phenytoin in tricyclic antidepressant-induced cardiotoxicity? Clin Toxicol (Phila). 2010 May;48(4):325-30. doi: 10.3109/15563650.2010.487050.
26. PMID: 27608281. Gosselin S, et al. Evidence-based recommendations on the use of intravenous lipid emulsion therapy in poisoning. Clin Toxicol (Phila). 2016 Dec;54(10):899-923. doi: 10.1080/15563650.2016.1214275. Epub 2016 Sep 8.
27. PMID: 27121236. American College of Medical Toxicology. ACMT Position Statement: Guidance for the Use of Intravenous Lipid Emulsion. J Med Toxicol. 2017 Mar;13(1):124-125. doi: 10.1007/s13181-016-0550-z. Epub 2016 Apr 27. Erratum in: J Med Toxicol. 2016 Dec;12(4):416. doi: 10.1007/s13181-016-0554-8.
28. PMID: 15811881. Greene SL, Dargan PI, Jones AL. Acute poisoning: understanding 90% of cases in a nutshell. Postgrad Med J. 2005 Apr;81(954):204-16. doi: 10.1136/pgmj.2004.024794.
29. PMID: 26174744. Chen HY, Albertson TE, Olson KR. Treatment of drug-induced seizures. Br J Clin Pharmacol. 2016 Mar;81(3):412-9. doi: 10.1111/bcp.12720. Epub 2015 Sep 17.
30. PMID: 22309432. Emamhadi M, Mostafazadeh B, Hassanijirdehi M. Tricyclic antidepressant poisoning treated by magnesium sulfate: a randomized, clinical trial. Drug Chem Toxicol. 2012 Jul;35(3):300-3. doi: 10.3109/01480545.2011.614249. Epub 2012 Feb 7.





Add comment