12 November 2023 by Shahriar Lahouti.
CONTENTS
- Preface
- Rapid review
- Pharmacokinetics
- Clinical manifestations
- Differential diagnosis
- Evaluation
- Management
- Going further
- References
Preface
Lithium is a commonly prescribed treatment for bipolar affective disorder. However, treatment is complicated by lithium’s narrow therapeutic index and its influence on kidney function, both of which increase the risk of toxicity. Lithium toxicity can affect multiple organs; with the central nervous system being the primary site of toxicity. Despite low mortality (~1% *), lithium intoxication may require intensive management over several days, and treatment decisions can be complex. Timely interventions such as fluid resuscitation and enhanced elimination in selected patients could reduce the risk of permanent neurological sequelae.
Rapid review
Pharmacokinetics
- Formulation: Lithium is available as an immediate release (IR) or a sustained release (SR) formulation.
- IR products are rapidly absorbed from the GI tract, and peak serum concentrations are achieved within 1-2 hours.
- SR products demonstrate a delay to peak of 4-6 hours.
- Distribution
- Lithium has no protein binding and distributes freely in total body water.
- The volume of distribution (Vd) is ~ 0.6- 0.9 L/kg *.
- The tissue distribution of lithium is a complex phenomenon, with a significant delay to achieve a steady state, similar to digoxin.
- The distribution into the brain can take up to 24 hours to reach equilibrium.
- Steady-state serum concentrations are typically reached within 5 days at the usual oral dose of 1200-1800 mg/day.
- Each 300 mg lithium carbonate tablet contains 8.12 mEq of lithium.
- Ingestion of a single 300-mg tablet is expected to increase the serum lithium level by ~ 0.1mEq/L (assuming a Vd of 0.6–0.9 L/kg and a patient weight of 50–100 kg) *.
- Lithium has no protein binding and distributes freely in total body water.
- Elimination
- Lithium is not metabolized and is cleared almost entirely by the kidneys.
- Lithium is handled by the kidneys much in the same way as sodium.
- It is freely filtered, and more than 80% is reabsorbed by the proximal tubule.
- There is also a small amount of reabsorption in the loop of Henle and the distal tubule.
- Lithium is handled by the kidneys much in the same way as sodium.
- The half-life for lithium is ~18h in adults and 36h in older adults *.
- Lithium is not metabolized and is cleared almost entirely by the kidneys.
Clinical manifestations
Gastrointestinal
- Nausea/vomiting, ileus
- Diarrhea
Neurologic: Lithium primarily is a neurotoxin.
- Movement disorder: Neuromuscular excitability
- Tremor (27%): The most common movement disorder.
- Fine tremor
- A fine action tremor is common in patients taking lithium at therapeutic doses. It can develop at any time during treatment.
- The fine tremor diminishes over time with continued therapy but increases with toxicity (coarse tremor)
- Generally, It is symmetric, limited to the arms, and nonprogressive.
- Coarse tremors
- It develops from lithium toxicity and is more disabling.
- It may also affect the legs and occur with other symptoms of toxicity.
- Fine tremor
- Ataxia/dysarthria, nystagmus, choreiform movements.
- Fasciculations.
- Myoclonus, hyperreflexia.
- Tremor (27%): The most common movement disorder.
- Altered mental status
- Delirium
- Seizure, nonconvulsive status epilepticus.
- Coma
| Syndrome of irreversible lithium-effectuated neurotoxicity (SILENT) * 🔸It is a potentially permanent neurologic injury resulting from lithium toxicity. 🔸SILENT is more common with chronic intoxication than acute toxicity. 🔸Cerebellar findings predominate in patients with SILENT. 🔸 In patients with Li intoxication, hyperthermia is a potential predictor for the development of SILENT. ♦️Although dialysis is a treatment for lithium poisoning, studies do not support that dialysis necessarily prevents SILENT. |
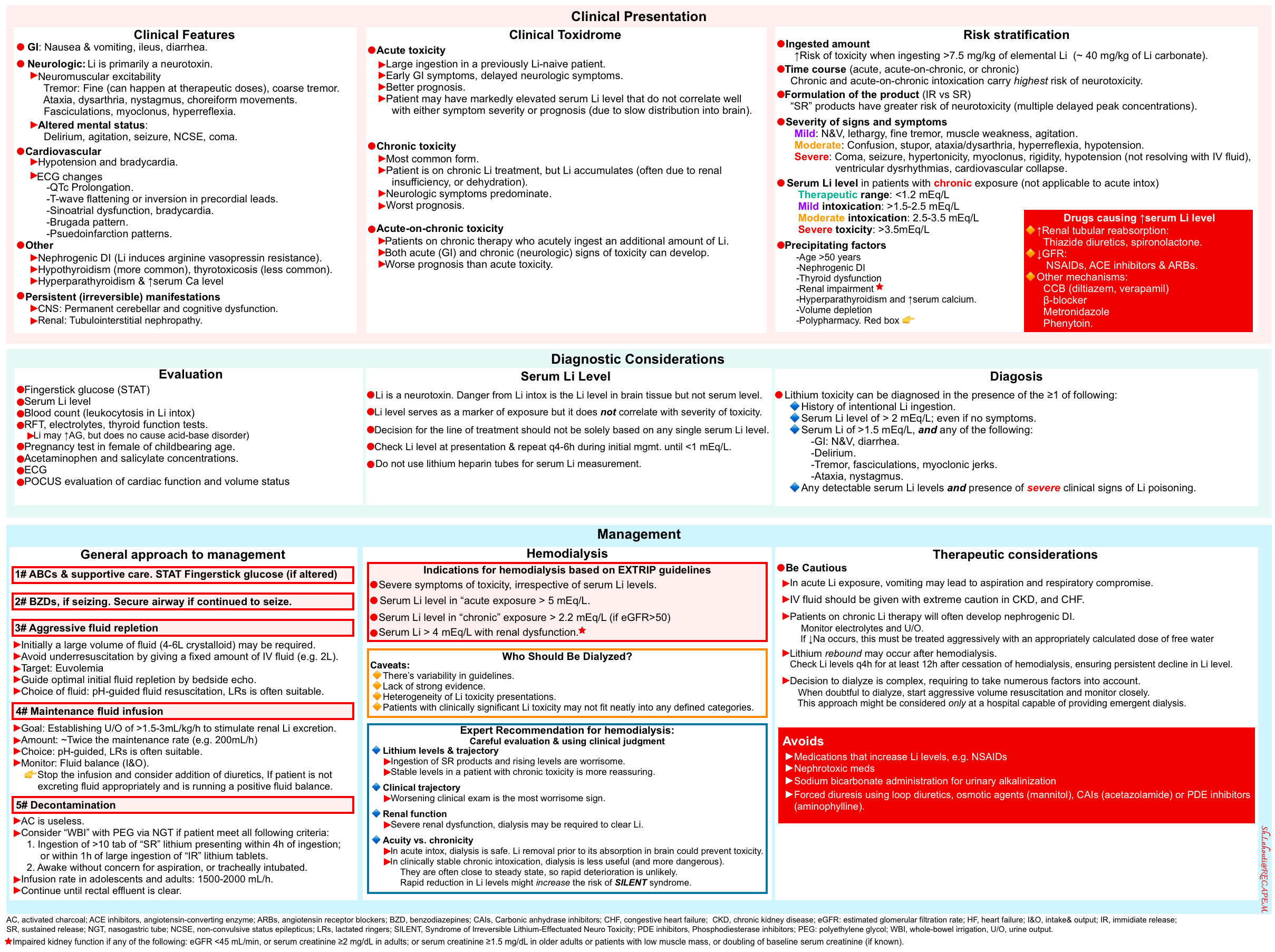
Cardiovascular
- Hypotension and bradycardia
- ECG:
- QTc prolongation
- Brugada phenocopy
-
- Lithium has a sodium channel blockade effect explaining some of the cardiovascular effects of lithium toxicity.
-
- T-wave flattening and inversion in precordial leads
- Sinoatrial dysfunction and bradycardia
- Pseudoinfarction patterns
Others
- Diabetes insipidus (DI)
- Thyroid: Both hypothyroidism and thyrotoxicosis.
- Hyperparathyroidism and hypercalcemia
Chronicity of exposure
Patients presenting with lithium toxicity will manifest different signs and symptoms based on the chronicity of their ingestion. Generally, there are 3 forms of lithium intoxication *:
- Acute
- This occurs when patients not taking lithium regularly ingest a large amount of lithium.
- Gastrointestinal symptoms predominate, and neurologic symptoms are delayed (because the Li redistributes slowly into the CNS from the serum).
- Patients may have high serum Li levels despite the absence of signs and symptoms of neurotoxicity.
- This form of toxicity generally carries less risk, and patients tend to have milder symptoms because the elimination half-life is shorter in patients who have never taken lithium.
- Chronic
- This is the most common form of intoxication and it happens in patients on chronic lithium doses, but lithium accumulates.
- Common causes of lithium retention include
- Renal insufficiency
- Dehydration
- Lithium-induced nephrogenic diabetes insipidus.
- Polypharmacy: use of diuretics (particularly thiazides), NSAIDs, or angiotensin-converting enzyme (ACE) inhibitors
- Common causes of lithium retention include
- The neurologic symptoms are predominant, and GI symptoms are typically absent.
- This mode of intoxication is associated with an increased risk of neurotoxicity.
- This is the most common form of intoxication and it happens in patients on chronic lithium doses, but lithium accumulates.
- Acute-on-chronic
- This occurs after an overdose ingestion in the setting of chronic lithium use.
- These ingestions may be more serious than acute ingestion because body tissues are already saturated with lithium, before the acute ingestion. With tissue saturation, any additional lithium leads to signs and symptoms of toxicity *.
- Both GI and neurologic signs and symptoms of toxicity are present.
Differential diagnosis
The differential diagnosis includes illnesses that cause vomiting and diarrhea and those that cause altered mental status and neuromuscular excitability.
DDx of neuromuscular excitability
- In patients with neuromuscular excitability who take psychiatric medications, the differential diagnosis includes:
- Neuroleptic malignant syndrome (NMS)
- NMS is characterized by bradykinesia and “lead pipe” rigidity while serotonin syndrome and lithium toxicity are both hyperkinetic (ie, tremor, myoclonus) *.
- Serotonin syndrome
- Overlap exists between the clinical symptoms of lithium toxicity and serotonin syndrome.
- Moreover, lithium can precipitate serotonin syndrome when taken in combination with other serotonergic medications *.
- However, definitively distinguishing Li toxicity from serotonin syndrome is not essential since management of both can occur concurrently (e.g. cessation of precipitating medications, control of neuromuscular excitability and hyperpyrexia, IV fluids).
- Neuroleptic malignant syndrome (NMS)
- Other important diagnoses to consider in patients who present with ataxia, altered mental status, or neuromuscular excitability include:
- Sympathomimetic intoxication (e.g. amphetamines, cocaine, pseudoephedrine)
- Withdrawals: Alcohol, benzodiazepine, baclofen *.
- Medications and intoxications that cause seizures and non-convulsive status epilepticus *
- Psychiatric medications (antipsychotics e.g. clozapine; antidepressants, especially bupropion or tricyclics).
- Selected opioids (meperidine, tramadol, propoxyphene)
- Methylxanthines (theophylline, caffeine)
- Local anesthetics (e.g. lidocaine, bupivacaine).
- Ketamine
- Baclofen
- Antihistamines
- Antiarrhythmics (e.g. procainamide, propranolol overdose)
- Antimicrobials (e.g. beta-lactams especially imipenem; quinolones; metronidazole; acyclovir; isoniazid).
- Chemotherapeutics & immunomodulator (e.g. methotrexate, chlorambucil, cyclosporine, tacrolimus)
- Nontoxicologic causes of seizures
- Brain disorders: CNS infections, head trauma, stroke.
- Hypoglycemia
- Myxedema coma or thyrotoxicosis
Evaluation
History
- Amount of ingestion
- Time of ingestion
- Formulation (i.e. IR vs. SR)
- Comorbidities
- Volume status: history of nausea/vomiting, diarrhea, adequacy of fluid intake, diuretic use
- Polypharmacy. Especially pay attention to agents that could affect lithium clearance.
- Potential coingestants
Labs *
- Fingerstick glucose (STAT)
- Serum lithium level
- Renal function test and electrolytes.
- Lithium intoxication may cause an increased anion gap but does not cause acid-base disturbances.
- Thyroid function tests
- Cell count
- Lithium intoxication can cause leukocytosis.
- Pregnancy test in women of childbearing age
- Acetaminophen and salicylate levels
- ECG
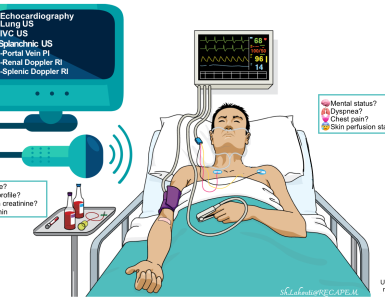
- POCUS evaluating cardiac function and volume status
Plasma Lithium Concentrations
- Therapeutic index of lithium is narrow.
- The target plasma concentration during initiation (e.g. acute mania) is 0.6 to 1.2 mEq/L.
- Serum lithium level
- When to obtain measurements?
- Whenever a patient on lithium is admitted to the hospital, or whenever lithium intoxication is a possibility.
- Sample collection
- Lithium must be measured in a lithium-free tube. Some blood tubes (green-top tubes) are treated with lithium heparin, which can cause falsely elevated
lithium concentrations *.
- Lithium must be measured in a lithium-free tube. Some blood tubes (green-top tubes) are treated with lithium heparin, which can cause falsely elevated
- Interpreting serum lithium level
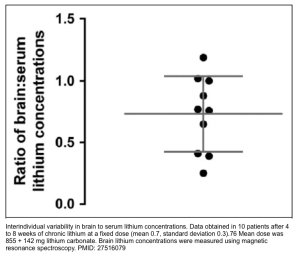
- The danger of lithium toxicity depends on total brain levels but not often the serum levels. Serum levels do not always correlate well with the degree of toxicity *.
- In acute intoxication, patients may have high blood levels with less severe symptoms.
- In chronic intoxication, patients can have more severe symptoms at a lower serum lithium level.
- Serum Li levels correlate more closely with the severity of clinical signs in patients with chronic toxicity because drug distribution has reached a steady state.
- However, even among patients on chronic Li therapy, the relationship between serum and brain lithium levels is poor (shown below) *.
- The danger of lithium toxicity depends on total brain levels but not often the serum levels. Serum levels do not always correlate well with the degree of toxicity *.
- When to obtain measurements?
-
- Diagnostic and therapeutic utility
- Early concentrations can help confirm “exposure” but may not represent peak serum concentrations especially, in a patient who has ingested sustained-release tablets.
- Serum Li levels are just one tool in the assessment of the severity of an overdose and may help to determine the need for hemodialysis.
- How often should it be measured?
- In acute or acute-on-chronic ingestion, lithium levels should be followed over time.
- Lithium levels should be repeated (every q4-6h initially) to determine:
- The adequacy of therapy (IV fluid or hemodialysis).
- Continued absorption, and distribution.
- Peak serum concentrations in a patient who has ingested sustained-release tablets.
- Once levels approach the therapeutic range or are consistently trending downwards, and the patient is improving clinically, serum lithium levels may be obtained less frequently (e.g. every 6-12 hours) until symptoms resolve.
- Diagnostic and therapeutic utility
Diagnosis
Lithium toxicity can be diagnosed in the presence of ≥1 of the following:
- History of intentional Li ingestion.
- Serum Li level of > 2 mEq/L; even if no symptoms.
- Serum Li of >1.5 mEq/L, and any of the following:
- GI: N&V, diarrhea.
- Delirium.
- Tremor, fasciculations, myoclonic jerks.
- Ataxia, nystagmus.
- Any detectable serum Li levels and presence of severe clinical signs of Li poisoning.
Risk stratification
Anticipated toxic effects of any lithium exposure will depend on the dose, kidney function, volume status, and whether the patient takes lithium chronically *. A comprehensive assessment can risk stratify individuals who present with lithium poisoning and help determine the most appropriate approach to management. Factors to consider include *:
- The ingested amount
- ↑Risk of toxicity when ingesting >7.5 mg/kg of elemental Li (~ 40 mg/kg of Li carbonate).
- Time course (acute, acute-on-chronic, or chronic)
- Chronic and acute-on-chronic intoxication carries the highest risk of neurotoxicity.
- Formulation of the product (IR vs SR)
- Sustained release (SR) products have a greater risk of neurotoxicity (multiple delayed peak concentrations) relative to immediate release (IR) products *.
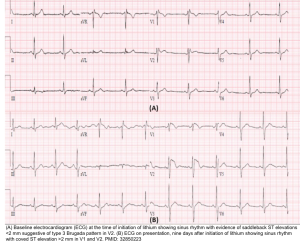
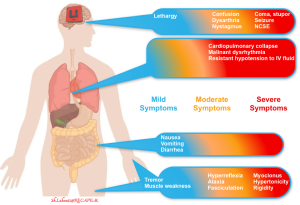
- Severity of signs and symptoms (figure below)
- 🔵Mild: N&V, lethargy, fine tremor, muscle weakness, agitation.
- 🟠Moderate: Confusion, stupor, ataxia/dysarthria, hyperreflexia, hypotension.
- 🔴Severe: Coma, seizure, hypertonicity, myoclonus, rigidity, hypotension (not resolving with IV fluid), ventricular dysrhythmias, cardiovascular collapse.
- Serum Li level in patients with chronic exposure (not applicable to acute intoxication)
- Therapeutic range: <1.2 mEq/L
- Mild intoxication: >1.5-2.5 mEq/L
- Moderate intoxication: 2.5-3.5 mEq/L
- Severe toxicity: >3.5mEq/L
- Personal factors (precipitating factors) *
- Age >50 years (adjusted odd ratio {OR} ~6) *
- Thyroid dysfunction (adjusted OR ~9) *
- Hypothyroidism is an independent risk factor for developing neurotoxicity in patients with chronic poisoning *.
- Hypothyroidism can cause a reduction in GFR and therefore reduced lithium elimination.
- Hyperthyroidism can increase lithium reabsorption thereby reducing lithium excretion.
- Hypothyroidism is an independent risk factor for developing neurotoxicity in patients with chronic poisoning *.
- Nephrogenic diabetes insipidus (adjusted OR ~26) *
- This predisposes the individual to volume depletion, in particular free water, with consequent activation of the renin–angiotensin aldosterone system which promotes lithium reabsorption.
- Renal impairment, if any of the following:
- eGFR <45 mL/min, or
- Serum creatinine ≥2 mg/dL in adults; or serum creatinine ≥1.5 mg/dL in older adults or patients with low muscle mass, or
- Doubling of baseline serum creatinine (if known).
- Hyperparathyroidism and ↑serum calcium
- This may lead to volume depletion secondary to the osmotic effects of hypercalcemia.
- Volume depletion
- Polypharmacy (causing ↑serum Li level) *
- ↑Renal tubular reabsorption: Thiazide diuretics, spironolactone.
- ↓GFR: NSAIDs, ACE inhibitors & ARBs.
- Other mechanisms: CCB (diltiazem, verapamil), β-blocker, metronidazole, phenytoin.
Severity of clinical signs and symptoms
Management
- The general approach to any poisoned patient begins with assessing and stabilizing the airway, breathing, and circulation (ABCs).
- Any patient with altered mental status should have a fingerstick glucose to exclude hypoglycemia.
- Benzodiazepines are first-line therapy for seizures.
- In a patient having continued seizures from suspected lithium toxicity, definitively secure the airway for the anticipated clinical course.
- Stop medications that can potentiate lithium toxicity (e.g. diuretics, NSAIDs) *.
GI decontamination
Activated charcoal (AC)
- Oral AC does not prevent the absorption of charged particles such as lithium and has no role in managing an isolated lithium ingestion.
Whole bowel irrigation (WBI) with polyethylene glycol (PEG) via NGT
- This should be considered if the patient meets all the following criteria *:
- Ingestion of >10 tabs of (SR) lithium presenting within 4h of ingestion; or within 1h of large ingestion of (IR) lithium tablets.
- Awake without concern for aspiration, or tracheally intubated.
- There is no benefit from whole-bowel irrigation in patients with chronic toxicity.
- Infusion rate in adolescents and adults: 1500-2000 mL/h, continued until the rectal effluent is clear.
- ⚠️Contraindication
- Ileus, bowel obstruction, or intestinal perforation.
- Hemodynamic instability (concern for sequestration of bowel and worsening of shock).
- Clinically significant GI bleeding.
- Intractable emesis.
- Altered mentation or lethargy unless the airway is protected.
Fluid and electrolytes
Background
- Lithium is eliminated by the kidney.
- Patients with lithium poisoning often have severe volume depletion.
- Those with acute intoxication usually have volume loss through vomiting or diarrhea.
- Patients with chronic lithium toxicity often are hypovolemic as the result of renal function impairment secondary to dehydration or overdiuresis.
- Many patients with lithium toxicity have volume-responsive decreases in kidney function.
- Monitoring for the development of hypernatremia in patients suspected of having nephrogenic DI is critical because this occurs in approximately 55% of patients on long-term lithium therapy.
- If hypernatremia is present, this must be treated aggressively with an appropriately calculated dose of free water (MDCalc).
Initial IV fluid resuscitation
- Patients often require large volumes of fluid resuscitation (e.g. 4-6L of crystalloid).
- Target: euvolemia
- Hemodynamic monitoring should guide fluid resuscitation (e.g., bedside echocardiography).
- Avoid underresuscitation by giving them a fixed dose of IV fluid e.g. 2L.
- Choice of the fluid: It might be selected based on the patient’s electrolytes, using the principles of pH-guided fluid resuscitation. In most situations, a Lactated Ringer is an appropriate choice.
Maintenance fluid infusion
- Goal: Establishing urine output of >1.5-3mL/kg/h to stimulate renal Li excretion.
- Amount: ~Twice the maintenance rate (e.g. 200mL/h)
- Choice: pH-guided, LRs often suitable.
- Monitor:
- Urine output (fluid balance).
- Stop the infusion and consider the addition of diuretics, If the patient is not excreting fluid appropriately and is running a positive fluid balance.
- Urine output (fluid balance).
Hemodialysis
Caveats
- Lithium is amenable to removal by hemodialysis; however, some characteristics of lithium make it difficult to remove, particularly in the setting of chronic toxicity.
- Lithium is predominantly localized intracellularly and diffuses slowly across cell membranes.
- When traditional intermittent hemodialysis is used for patients with chronic exposures, clearance of the blood compartment is often followed by a rebound phenomenon of redistribution from tissue stores, leading to recurrent increased serum concentrations.
- Moreover, the “target organ” of toxicity, the brain, is not directly affected by hemodialysis but depends upon redistribution between compartments for clearance.
- Lithium is predominantly localized intracellularly and diffuses slowly across cell membranes.
- In patients on chronic lithium use, rapidly dropping the lithium level might increase the risk of chronic neurologic injury *.
- There are no observational studies or randomized controlled trials regarding the use of hemodialysis in lithium toxicity *.
- This has caused a significant variability in clinical decision-making when it comes to using dialysis in the management of lithium poisoning.
When to dialyze
- More recently, the Extracorporeal Treatments in Poisoning Workgroup (ExTRIP) analyzed available data and suggested hemodialysis if any of the following conditions are present *:
- Severe symptoms of toxicity, irrespective of serum Li levels.
- Serum Li level in “acute” exposure > 5 mEq/L.
- Serum Li > 4 mEq/L with “renal dysfunction“.
- Impaired kidney function if any of the following:
- eGFR <45 mL/min, or serum creatinine ≥2mg/dL in adults; or serum creatinine ≥1.5 mg/dL in older adults or patients with low muscle mass, or doubling of baseline serum creatinine, if known. In children, serum creatinine is > 2 times the upper limit of normal for age and sex.
- Impaired kidney function if any of the following:
- If the expected time to obtain a serum lithium concentration <1 mEq/L with optimal management is more than 36 hours.
- In patients with symptoms suggestive of chronic lithium toxicity:
- A serum lithium concentration >1.8 mEq/L if eGFR <50 mL/min.
- Serum lithium concentration >2.2 mEq/L if eGFR >50 mL/min.
- However, dialysis decisions should be made in conjunction with a toxicologist. Several factors need to be considered when deciding whether to dialyze:
- Lithium levels and trajectory
- Rising levels and ingestion of sustained-release lithium may suggest that the intoxication will get worse before it gets better *.
- Stable levels in a patient with chronic toxicity suggest that the patient is unlikely to deteriorate suddenly.
- Clinical trajectory
- Signs and symptoms are helpful because they reflect the brain’s lithium level.
- Worsening clinical examination is potentially the most worrisome sign.
- Renal function
- In severe renal dysfunction, dialysis may be required to clear lithium *.
- Chronocity
- In acute Li intoxication, dialysis seems to be safe. Removal of lithium before its absorption in the brain could prevent toxicity.
- In patients with chronic Li toxicity who are clinically fine, dialysis is less helpful and may be more dangerous.
- As these patients are often close to a steady state, rapid clinical deterioration is unlikely.
- Rapid reduction in Li levels might increase the risk of SILENT syndrome in this context.
- Lithium levels and trajectory
| ✅A conservative approach can be considered when in doubt about whether to dialyze since the time course of Li intox is relatively long compared to other poisons, evolving over days *. 💡A reasonable approach is aggressive volume resuscitation and monitoring carefully with ongoing consultation with a toxicologist (this approach is applicable only at a hospital capable of providing emergent dialysis). |
Dialysis technique
- Intermittent hemodialysis (IHD) is the recommended methodology (although continuous methods are acceptable).
- Continuous renal replacement therapies (CRRTs)
- These include continuous venovenous hemodialysis and continuous venovenous hemodiafiltration.
- Indications:
- When IHD is not available.
- Hemodynamic instability.
- CRRT is associated with a reduced likelihood of rebound in plasma lithium concentrations but at the cost of a lower clearance compared with IHD *.
- Generally, it is recommended that CRRT requires 24 hours of continuous therapy to decrease lithium to a similar extent as that achieved from 4 hours of IHD, due to the slower clearance.
- Rebound effect
- Measure serum lithium level immediately after hemodialysis is completed and again 6h after dialysis to assess for the rebound effect.
- Lithium equilibrates slowly between the extracellular and intracellular fluid compartments. As a result, a rebound increase in serum lithium concentrations occurs after the cessation of hemodialysis, as intracellular lithium diffuses back into the extracellular space.
- Ongoing gastrointestinal drug absorption may also contribute to the rebound effect.
- A rebound in concentration may suggest that another session of dialysis is required.
- Measure serum lithium level immediately after hemodialysis is completed and again 6h after dialysis to assess for the rebound effect.
Going further
References
1. PMID: 27516079. Baird-Gunning J, Lea-Henry T, Hoegberg LCG, Gosselin S, Roberts DM. Lithium Poisoning. J Intensive Care Med. 2017 May;32(4):249-263. doi: 10.1177/0885066616651582. Epub 2016 Aug 11.
2. PMID: 3668585. Adityanjee. The syndrome of irreversible lithium effectuated neurotoxicity. J Neurol Neurosurg Psychiatry. 1987 Sep;50(9):1246-7. doi: 10.1136/jnnp.50.9.1246.
3. PMID: 20393430.Dunne FJ. Lithium toxicity: the importance of clinical signs. Br J Hosp Med (Lond). 2010 Apr;71(4):206-10. doi: 10.12968/hmed.2010.71.4.47513.
4. PMID: 30743298. Rajan S, Kaas B, Moukheiber E. Movement Disorders Emergencies. Semin Neurol. 2019 Feb;39(1):125-136. doi: 10.1055/s-0038-1677050. Epub 2019 Feb 11.
5. PMID: 31075831. Francescangeli J, Karamchandani K, Powell M, Bonavia A. The Serotonin Syndrome: From Molecular Mechanisms to Clinical Practice. Int J Mol Sci. 2019 May 9;20(9):2288. doi: 10.3390/ijms20092288.
6. PMID: 20717751. Ross JC, Cook AM, Stewart GL, Fahy BG. Acute intrathecal baclofen withdrawal: a brief review of treatment options. Neurocrit Care. 2011 Feb;14(1):103-8. doi: 10.1007/s12028-010-9422-6.
7. PMID: 19374461. Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach. Part II: Clinical pharmacology and therapeutic monitoring. CNS Drugs. 2009;23(4):331-49. doi: 10.2165/00023210-200923040-00005.
8. PMID: 34462294. Kobylianskii J, Austin E, Gold WL, Wu PE. A 54-year-old woman with chronic lithium toxicity. CMAJ. 2021 Aug 30;193(34):E1345-E1348. doi: 10.1503/cmaj.210725.
9. PMID: 11990895. Oakley PW, Whyte IM, Carter GL. Lithium toxicity: an iatrogenic problem in susceptible individuals. Aust N Z J Psychiatry. 2001 Dec;35(6):833-40. doi: 10.1046/j.1440-1614.2001.00963.x.
10. PMID: 7962676. Swartz CM, Jones P. Hyperlithemia correction and persistent delirium. J Clin Pharmacol. 1994 Aug;34(8):865-70. doi: 10.1002/j.1552-4604.1994.tb02053.x.
11. PMID: 25583292. Decker BS, et al. EXTRIP Workgroup. Extracorporeal Treatment for Lithium Poisoning: Systematic Review and Recommendations from the EXTRIP Workgroup. Clin J Am Soc Nephrol. 2015 May 7;10(5):875-87. doi: 10.2215/CJN.10021014. Epub 2015 Jan 12.
12.PMID: 24655138. Roberts DM, Gosselin S. Variability in the management of lithium poisoning. Semin Dial. 2014 Jul-Aug;27(4):390-4. doi: 10.1111/sdi.12235. Epub 2014 Mar 21.




Add comment