1 February 2023 by Shahriar Lahouti.
CONTENTS
- Preface
- Case scenario
- Pathophysiology
- Triggers and evaluation for the cause(s)
- Clinical presentation
- Diagnosis and differentials
- Management
- Appenidx
- Media
- Going further
- References
Preface
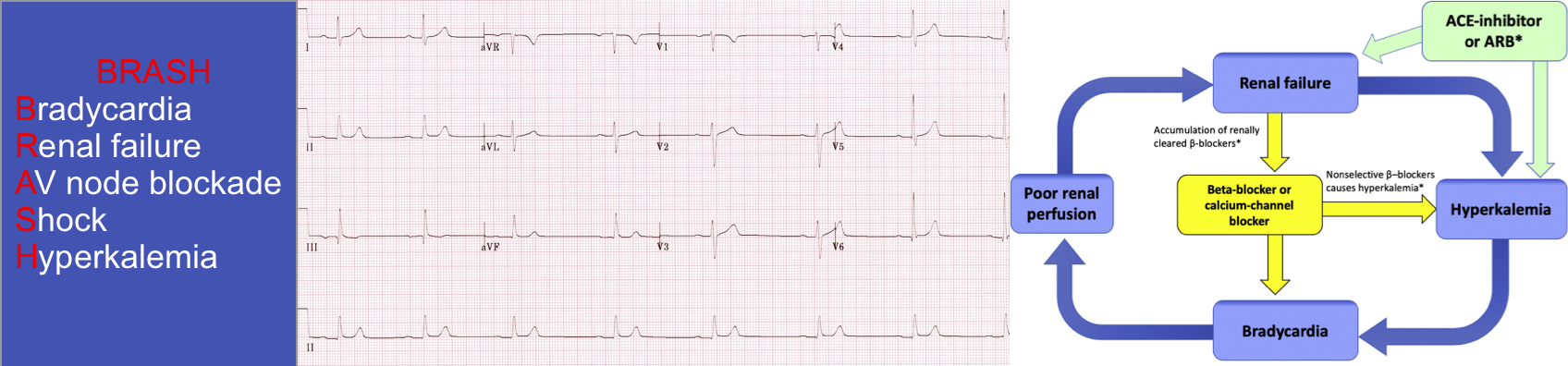
BRASH syndrome is a combination of Bradycardia, Renal failure, AV(atrioventricular) nodal blockade, Shock, and Hyperkalemia. It is clinically essential to take these manifestations as a syndrome rather than isolated findings because they are interrelated and have synergistic effects. The most common error in managing BRASH syndrome is focusing on a single component of the syndrome (e.g. hyperkalemia) meanwhile, other aspects of the syndrome are overlooked. Understanding and recognising the pathophysiology of BRASH syndrome as a distinct entity allow us to employ appropriate treatment plan which may improve patient outcomes.
Case scenario
A 65-years-old man presented to ER with generalized weakness, non-bloody diarrhea, vomiting, and low oral intake for the past 3 days. Upon examination, he was dehydrated, bradycardic up to 30 bpm, and hypotensive (70/40 mm Hg). He was mildly drowsy but oriented to time, place, and person. The rest of the physical examination was unremarkable. ECG was remarkable for bradycardia with a junctional rhythm.
- Past medical history: Stage 4 CKD (baseline creatinine 2.6 mg/dL), coronary artery disease, heart failure with low ejection fraction (25%), hypertension, and atrial fibrillation.
- Long-term medications: Bisoprolol 2.5mg OD, valsartan 80mg OD, furosemide 40mg OD, and spironolactone 12.5mg OD.
Patient was given a liter of fluid (because of low BP) before the labs return. Initial blood work results shows potassium 5.7 mmol/L. The creatinine 7.5 mg/dL, and a severe metabolic acidosis (pH of 6.9) with elevated anion gap to 38. Lactic acid was elevated (9.4mmol/L).
- We know how to treat bradycardia and hyperkalemia. Why is it important to consider BRASH as separate entity?
- How do you treat this patient?
Pathophysiology
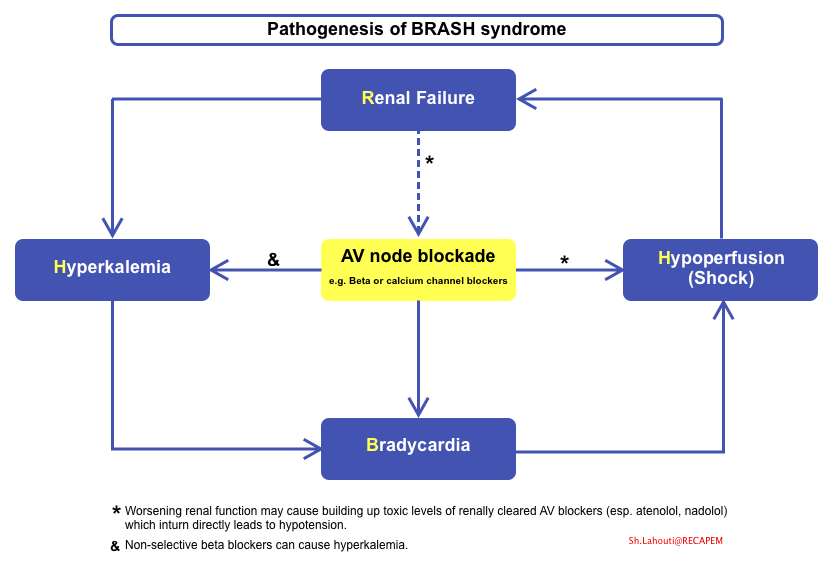
Josh Farkas proposed a pathophysiologic cycle of events leading to refractory bradycardia and renal dysfunction, which does not respond to the usual advanced cardiac life support (ACLS) resuscitation protocols *.
1# The core pathogenesis of BRASH syndrome: Synergistic bradycardia
- The severity of bradycardia is unexpected and is out of proportion to severity of hyperkalemia or AV blockade effect. Why?
- Findings in BRASH syndrome:
- Isolated hyperkalemia may cause bradycardia, generally when hyperkalemia is severe (e.g. potassium > 7 mEq/L). At this high potassium level other features of hyperkalemia on ECG (e.g. QRS widening) are often present. However in BRASH syndrome, hyperkalemia of often mild-moderate and ECG signs of hyperkalemia are absent.
- AV nodal blockade can cause bradycardia, however this effect is often not seen with therapeutic doses. Marked bradycardia in BRASH is present despite that patients were taking their medications as directed.
- Findings in BRASH syndrome:
- Having said that, the bradycardia in BRASH results from synergistic effect of hyperkalemia and AV nodal blockers.
2# The perpetual cycle of BRASH syndrome(figure below)
- Bradycardia can result in hypoperfusion, which can cause renal injury. The resultant renal injury causes hyperkalemia which potentiates the bradycardia.
- This spiral may be even more dramatic among patients who are taking beta blockers which are cleared by the kidneys (e.g. atenolol, nadolol, bisoprolol *). In that case, renal failure may cause beta blocker accumulation, further accelerating the vicious spiral.
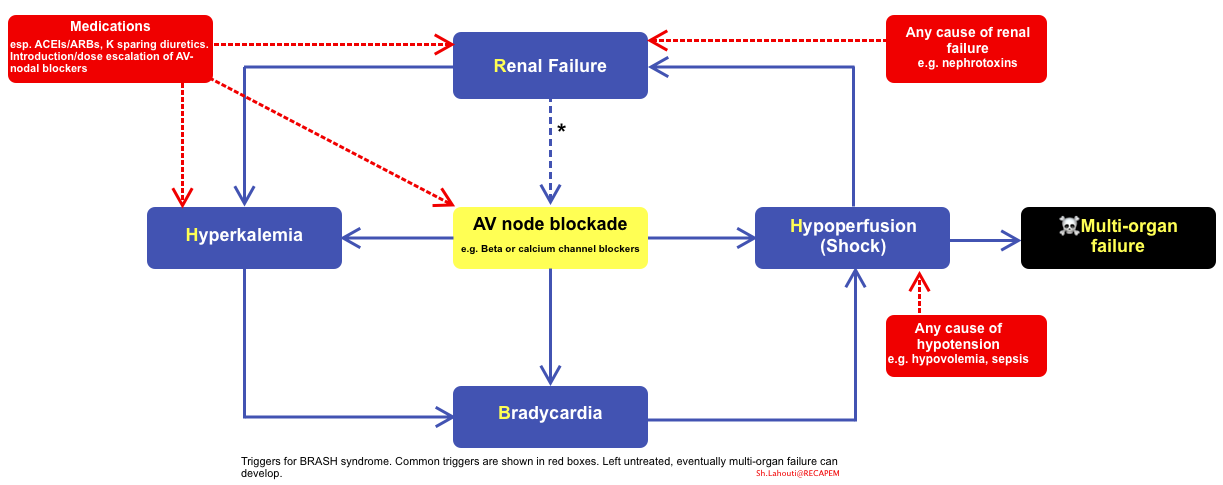
Triggers and evaluation for the causes
Triggers for the BRASH syndrome
- Any causes of renal failure (see more on this here).
- Example include shock of any etiology (esp. hypovolemia), hepatorenal syndrome, nephrotoxic medications, rhabdomyolysis , tumor lysis syndrome
- Any causes of hyperkalemia (more on this here).
- Example include potassium supplementation, medications such as ACEIs/ARBs, and potassium-sparing diuretics e.g. spironolactone.
- Dose escalation or introduction of AV nodal blocking medications
Evaluation for the underlying cause(s)
- It is important to remember that BRASH syndrome is a syndrome rather than a specific diagnosis. Therefore identifying BRASH syndrome is not enough.
- It is critical to understand why the patient developed BRASH syndrome.
- A thorough history and physicals and POCUS (to assess volume status) will usually disclose the cause of the BRASH syndrome.
- If the cause is unclear, evaluate for possible underlying causes:
- Evaluate for AKI: urinalysis, creatinine kinase, and renal ultrasound.
- Infectious: Cultures
- MI: Troponin (if clinically indicated)
Clinical presentation
BRASH syndrome is common among elderly patients with hypertension, atrial fibrillation, CKD; and those patients who use AV nodal blockers (BB, CCB), ACEIs/ARBS or potassium sparing diuretics *.
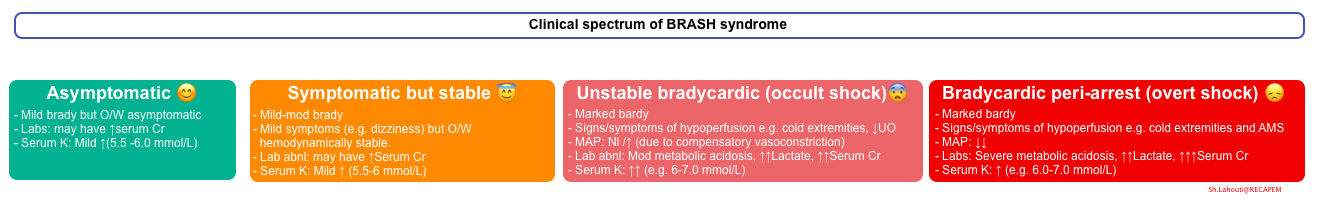
Clinical presentation of patients with BRASH syndrome is variable (shown below). Some patients present with asymptomatic laboratory abnormalities, while other patients can present with cardiogenic shock and multiple organ failure. However the dominant feature of any patient with BRASH syndrome falls into two categories:
- Marked bradycardia and hypotension with only mild hyperkalemia (e.g. 5.5-6 mmol/L).
- Severe hyperkalemia (6-7.5 mmol/L) with only moderate bradycardia and preserved blood pressure.
Diagnosis and differentials
Diagnosis
- Remember that BRASH is a syndrome, not a single disease entity.
- Diagnosis can be simply made, based on patient’s medication list, vital signs, and basic laboratory data.
- BRASH should be considered among all patients with bradycardia.
- Look for the serum potassium?
- If the patient is hyperkalemic (even mild), look for AV nodal blocker medications and renal failure.
- Note that even if they don’t have the complete syndrome, the hyperkalemia needs to be treated.
Differential diagnosis
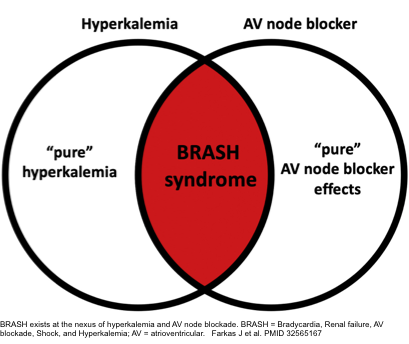
- The most important distinction to made is whether the presentation is due to isolated hyperkalemia, or from AV blocker intoxication. In practice, sometimes these entities are along a continuum which at times may be impossible to parse out.
- Some key distinctions are as follows:
- BRASH vs. isolated hyperkalemia
- When hyperkalemia is driving the clinical presentation, the serum K is > 7-7.5 mmol/L and significant ECG changes (e.g. QRS widening) are present *.
- BRASH syndrome often have mild-moderate hyperkalemia (6-7 mmol/L) and significant ECG changes are often absent.
- Presence of acute kidney injury (or AKI on top of CKD) and bradycardia suggest a constellation of BRASH syndrome, rather than isolated hyperkalemia.
- BRASH syndrome versus AV blocker intoxication
- When clinical presentation is primarily driven by AV blocker intoxication, serum K is usually normal. Patients frequently report recent use of a new medication or dose escalation *.
- BRASH vs. isolated hyperkalemia
Management
The most common error in managing BRASH syndrome is fixating on a single component of the syndrome (e.g. hyperkalemia) and focusing solely on management of that problem (e.g. emergent dialysis). Meanwhile, other aspects of the syndrome are overlooked (e.g. the patient might remain under-resuscitated, bradycardic, and malperfused). Identifying BRASH is important because it reminds us to treat all of the involved parts *.
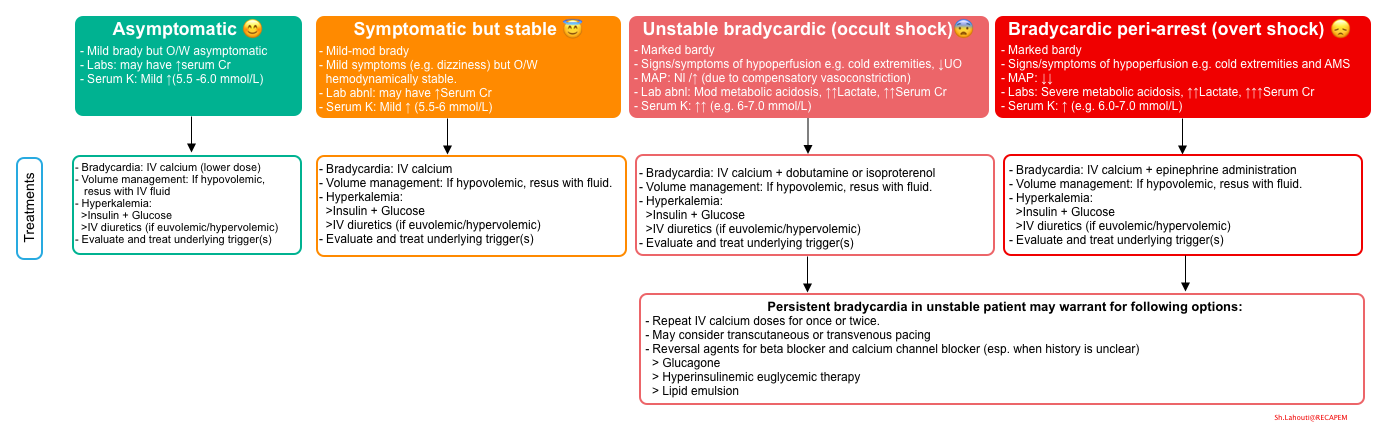
- Since BRASH is a syndrome, simultaneous treatment of each components of the syndrome should be performed. This include
- Treatment of hypoperfusion
- Management of bradycardia.
- Optimizing MAP and renal perfusion pressure
- Volume management (if necessary).
- Using inotrope and/or chronotrope medications (if warranted) to improve organ perfusion pressure.
- Treatment of hyperkalemia
- Identify and treat any underlying cause(s)
- Treatment of hypoperfusion
The simultaneous treatment of each component of BRASH syndrome for the spectrum of clinical presentation is summarized below.
| Volume management |
- Volume status varies widely among patients with BRASH syndrome from volume depleted (more common) to those with volume overload with systemic congestion.
- Volume assessment
- POCUS: Lung, heart, IVC
- History: Poor oral intake, GI loss, bleeding, overdiuresis, recent weight loss, non-adherent to diet and medications?
- Exam: Peripheral edema, pleural effusion, ascites?
- Volume management
- Optimizing volume status improve renal perfusion and is prerequisite for effective kaliuresis (below).
- Hypovolemic patients: Choose a fluid which will treat pH abnormalities (pH-guided resuscitation). See appendix for different features of volume expanders. The amount of given volume should be individualized.
- Isotonic bicarbonate: Patients with non-anion gap metabolic acidosis and uremic acidosis may benefit from isotonic bicarbonate.
- Lactated Ringers: For volume depletion and a normal acid-base status.
- 0.9% saline: May be preferred in patients with metabolic alkalosis.
- Albumin: patients with hepatorenal syndrome.
- Hypervolemia
- Diuretic: For patients who are initially hypervolemic, diuresis alone may be used to control both hyperkalemia and volume overload. See below.
| Bradycardia |
- The significance of bradycardia effect on cardiac output is discussed here.
- 🎗Reminder
- Patients with marked bradycardia (e.g. HR < 30 bpm) may presents with signs and symptoms of hypoperfusion (e.g. cold extremities) despite normal or even high BP (occult bradycardic shock).
- In these patients compensatory vasoconstrictor response may maintain BP and mental status despite the low cardiac output and poor organ perfusion.
- If occult bradycardic shock is not recognized and urgently managed, overt bradycardic shock with frank hypotension and organ hypoperfusion develops.
- Patients with marked bradycardia (e.g. HR < 30 bpm) may presents with signs and symptoms of hypoperfusion (e.g. cold extremities) despite normal or even high BP (occult bradycardic shock).
- Bradycardia in the context of BRASH syndrome is caused by synergistic effects of hyperkalemia and AV nodal blockers. Having said that, the initial treatment of choice include:
- IV Calcium
- Epinephrine
- Dobutamine or Isoproterenol
- IV Calcium
- Counteract the effect of hyperkalemia on myocardium and may also work as an antidote to AV nodal agents.
- Initial dose: Give calcium chloride 1g (ideally via central line) or calcium gluconate 3g (via peripheral line).
- Note that the dosage depend on severity of hyperkalemia. Patients with less sever hyperkalemia may require lower doses of calcium while patients with more severe hyperkalemia and “multiple” ECG changes (beyond bradycardia, e.g. QRS widening) require higher doses with repeated doses of calcium.
- Remember that IV calcium lasts only 30-60 minutes, so it may need to be repeated.
- In cases of persistent bradycardia, the initial dose may be repeated once or twice.
- Epinephrine
- For bradycardic patients with frank hypotension, epinephrine is the best choice.
- Epinephrine increase the HR and vascular tone. It stimulates beta-2 receptors, causing potassium to shift inside cells.
- It is safe to give via peripheral line.
- Dosage:
- ~ 20-50 mcg IV bolus dose followed by 2-10 mcg/min infusion. See appendix for preparing Epi Drip.
- ~ 20-50 mcg IV bolus dose followed by 2-10 mcg/min infusion. See appendix for preparing Epi Drip.
- Dobutamine or isoproterenol
- These are more suitable agents in patients with occult bradycardic shock (recognized by marked bardycardia, cold extremities/poor urine output despite normal or even high BP).
- It is important to identify and treat occult bradycardic shock since if left untreated, it may cause renal hypoperfusion and diuretic unresponsiveness.
- Unlike epinephrine, these two beta agonists lack any alpha-agonist (vasoconstrictive) properties.
- Therefore, they are suitable for a patient with occult bradycardic shock who benefit more from a pure chronotrope while avoiding hypertension.
- These are more suitable agents in patients with occult bradycardic shock (recognized by marked bardycardia, cold extremities/poor urine output despite normal or even high BP).
- Pacing (transvenous or transcutaneous)
- May be indicated for hemodynamically unstable bradycardia which is refractory to medical therapies.
- Atropine?
- Is not an effective agent for bradycardia. More on this, here
- Moreover, in the context of hyperkalemia, atropine doesn’t shift potassium into the cells (as beta agnosits do).
- Antidotes for calcium channel blockers or beta blockers?
- Multidimensional treatment of BRASH syndrome is frequently effective and these agents are not required. These agents are usually reserved for intoxication with calcium channel blockers or beta blockers.
- However, in unclear conditions where the patient isn’t responding to any other therapy, they might nonetheless be considered.
| Hyperkalemia |
- Treatment options for hyperkalemia is discussed here.
- Temporary management
- Insulin: 5 units IV bolus
- Dextrose:
- If glucose > 250 mg/dL: No need for initial dose
- If glucose 180-250 mg/dL: Give 25g glucose (1 amp of D50W)
- If glucose <180 mg/dL: Give 50g of glucose (2 ampules of D50W)
- The effect will last for 4-6h. This may be repeated every 2-4hours, with serial monitoring of blood glucose levels.
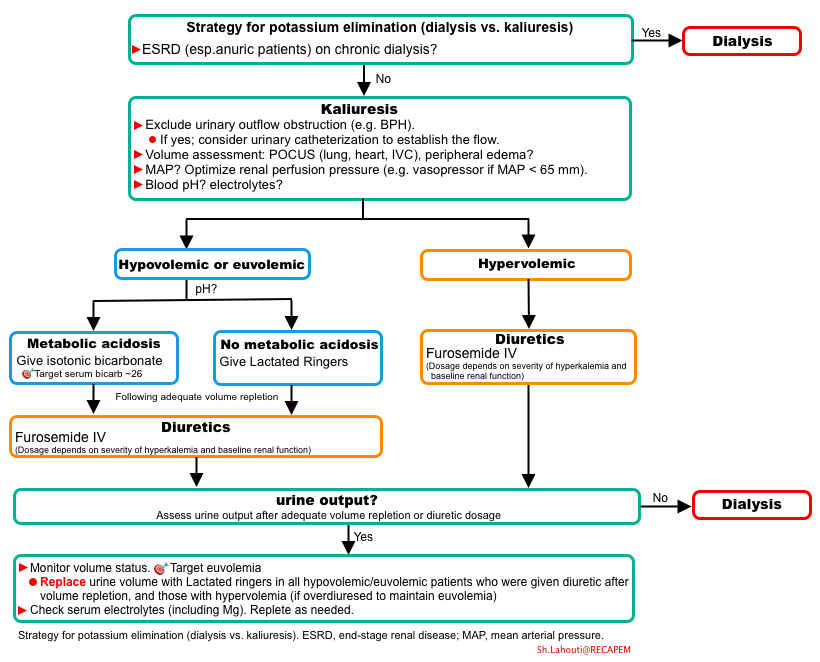
- Potassium elimination
- Eventually, hyperkalemic patients require elimination of excess potassium from the body which can be achieved either through the kidney (kaliuresis) or by dialysis.
- For most patients (except those with ESRD on chronic dialysis), kaliuresis should be attempted prior to emergent dialysis.
- Establishment of effective kaliuresis involves appropriate renal perfusion pressure, volume resuscitation or diuretic administration.
- ⚠️Diuretics alone will often fail if the patient is under-resuscitated and malperfused.
- Diuretic dosage
- Factors affecting how aggressive to be in treatment of hyperkalemia
- The severity of the hyperkalemia.
- The degree of renal insufficiency (more severe renal failure will make it harder to treat the hyperkalemia). For example:
- Patients with preserved renal function: Furosemide 40mg IV q12h.
- Mild-moderate renal insufficiency: Furosemide 60-120mg IV q12h
- Severe renal function impairment (eGFR<30): May require 160mg IV q12h.
- The amount of isotonic bicarbonate required (isotonic bicarbonate will draw down the potassium, so patients who require resuscitation with isotonic bicarbonate may require less aggressive therapy for hyperkalemia).
- Based on the above variables, treatment of hyperkalemia will vary quite a bit. For example:
- In a patient with mild/moderate hyperkalemia and mild kidney injury, a few doses of furosemide are sufficient.
- In a patient with severe hyperkalemia and severe renal injury, multiple high doses of diuretic may be needed.
- Factors affecting how aggressive to be in treatment of hyperkalemia
Algorithm
Strategy for potassium elimination
RECAP
- BRASH syndrome is often misdiagnosed as isolated hyperkalemia or isolated bradycardia. This will contribute to focusing on management of a single component of the syndrome, leading to a failure to treat the entire syndrome.
- The key to BRASH is recognizing all the components and treating them simultaneously.
- Standard ACLS strategies for bradycardia may fail to work in patients with BRASH syndrome, since they don’t incorporate the use of IV calcium *.
- Failure to identify and promptly manage the patients with unstable bradycardia leads to end-organ hypoperfusion and dysfunction. These patients deserve rapid restoration of HR and perfusion pressure (which often requires epinephrine or dobutamine) even if the BP superficially looks fine.
- In patients who are under-resuscitated (poor perfusion pressure), diuretic alone will fail to provide proper kaliuresis.
Appendix
Comparison of volume expanders
Media
Going further
References
1. Farkas JD, Long B, Koyfman A, Menson K. BRASH Syndrome: Bradycardia, Renal Failure, AV Blockade, Shock, and Hyperkalemia. J Emerg Med. 2020 Aug;59(2):216-223. doi: 10.1016/j.jemermed.2020.05.001. Epub 2020 Jun 18. PMID: 32565167.






Add comment