25 June, 2023 by Shahriar Lahouti. Last update 1 December 2024.
CONTENTS
- Preface
- Pathophysiology
- Epidemiology and causes
- Clinical presentation and diagnosis
- Differential diagnosis
- Other diagnostic evaluation
- General approach to critical patients
- Initial therapeutic options in ED
- Special contions
- RECAP
- Appendix
- Media
- References
Preface
Pneumothorax is a common and potentially life-threatening clinical condition that may require emergency treatment in the ED. Tension pneumothorax is a medical emergency and requires a high index of suspicion, prompt recognition, and intervention. The provider needs to be familiar with the pathophysiology, and wide array of etiologies when faced with pneumothorax so that appropriate therapy can be administered promptly to prevent deterioration and recurrence. In this post, a comprehensive approach to the diagnosis and management of pneumothorax is discussed in view of the most recent literature.
Pathophysiology
From the pathophysiologic point of view, pneumothoraces can be classified as simple, tension. A simple pneumothorax does not have a tension physiology.
| Simple pneumothorax |
Mechanism
- Pneumothorax arises when free air enters the potential space between the visceral and parietal lung pleura. Air can enter the pleural space by two main routes *
- Communication between alveoli and pleura.
- Communication (direct or indirect) between atmosphere and pleura.
- The air accumulation can apply pressure on the lung and make it collapse.
Spectrum of clinical presentation
- The severity of signs and symptoms depends on several pathophysiologic factors including:
- Size of pneumothorax
- Generally, a larger pneumothorax is more likely to cause respiratory compromise and hypoxia.
- Note that the size of the pneumothorax can change over time as
- Resolving pneumothorax
- Static
- Expanding
- Cardiopulmonary reserve
- A patient with underlying lung disease (e.g. pulmonary fibrosis) is more prone to develop respiratory distress and hypoxia due to a smaller pneumothorax compared to a patient with healthy lungs.
- Size of pneumothorax
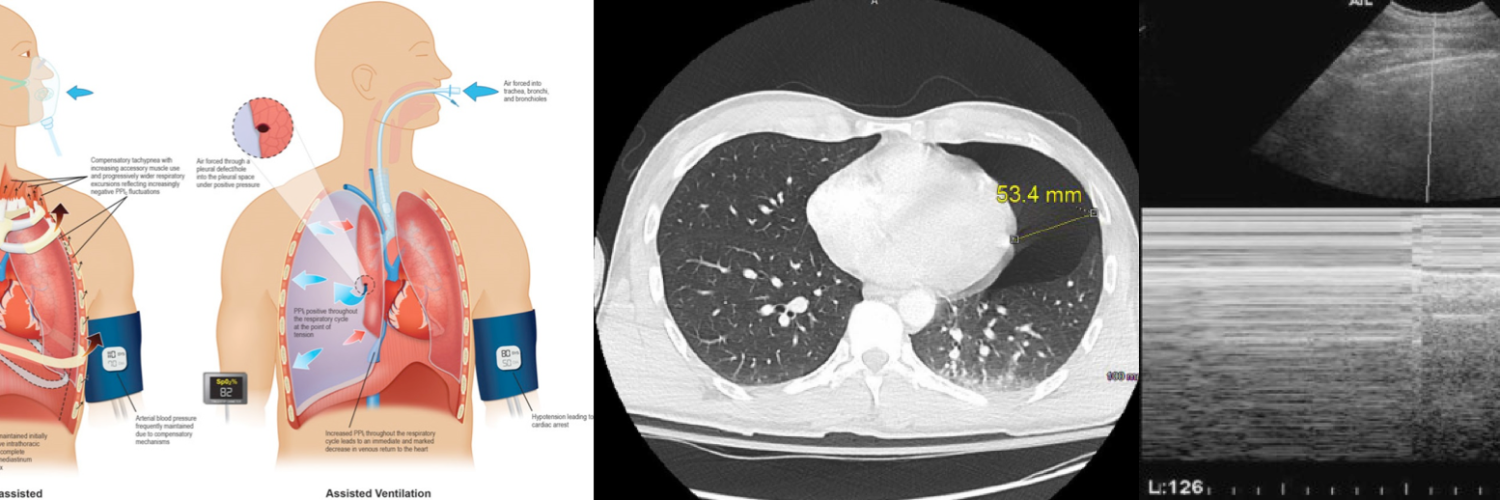
| Tension pneumothorax (TPT) |
Mechanism
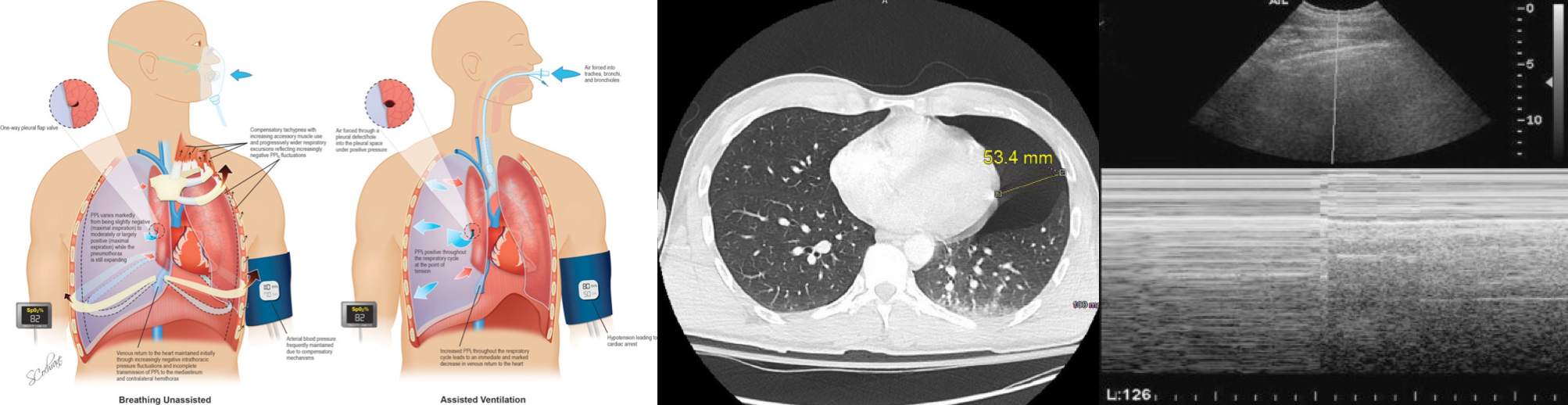
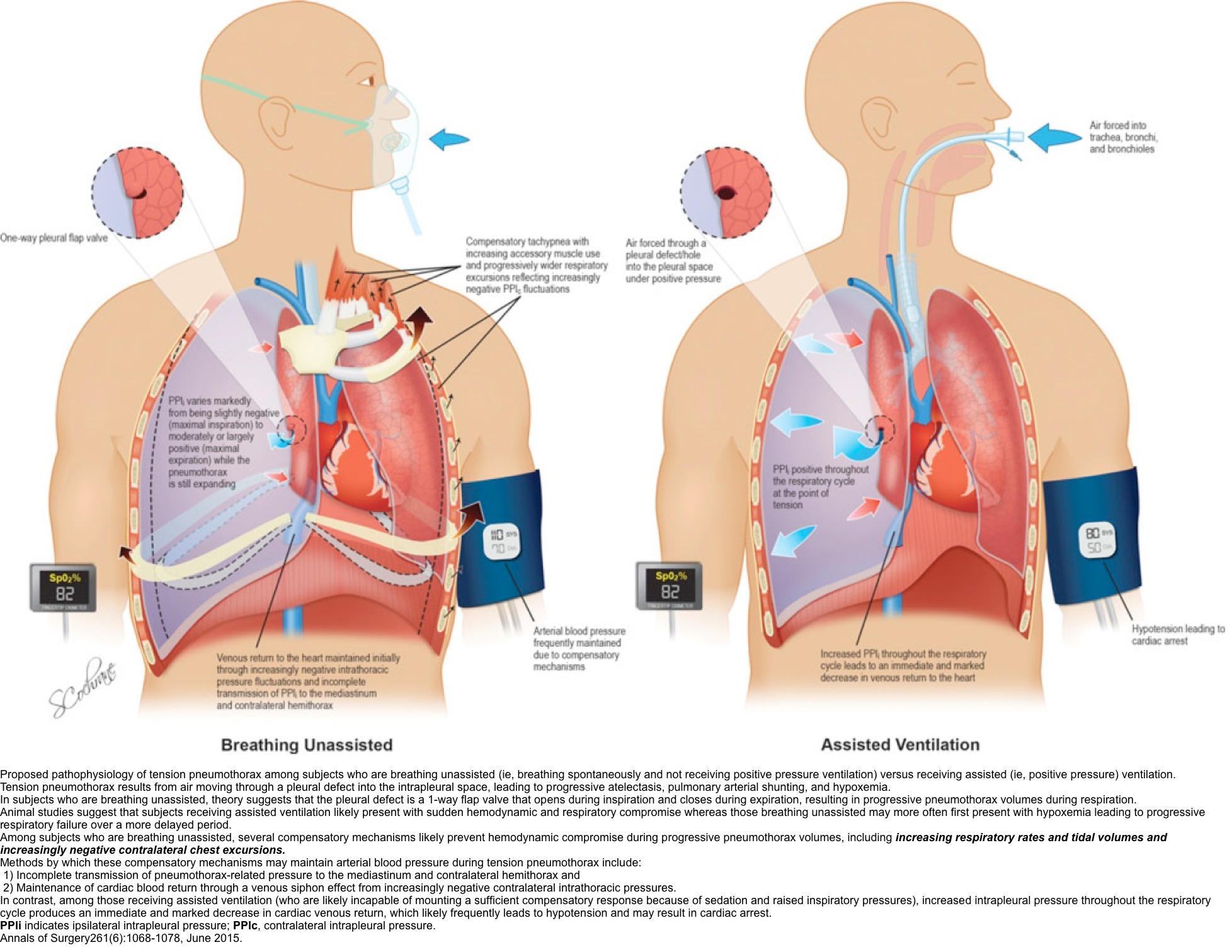
- The mechanism that creates tension physiology has been postulated in two groups of patients:
- In spontaneously breathing patients
- The pleural defect functions as a one-way valve, allowing the air to enter the pleural cavity on inspiration but does not allow the air to exit on expiration. This causes increasing positive intrapleural pressure *.
- The progressively rising intrapleural pressure causes further ipsilateral lung collapse and exerts a mass effect on the contralateral lung and possibly mediastinum (compression of vessels and heart).
- In patients on assisted ventilation (positive pressure ventilation)
- Air is forced into the pleural cavity through a pleural defect during the whole respiratory cycle under positive pressure.
- In spontaneously breathing patients
Spectrum of clinical presentation
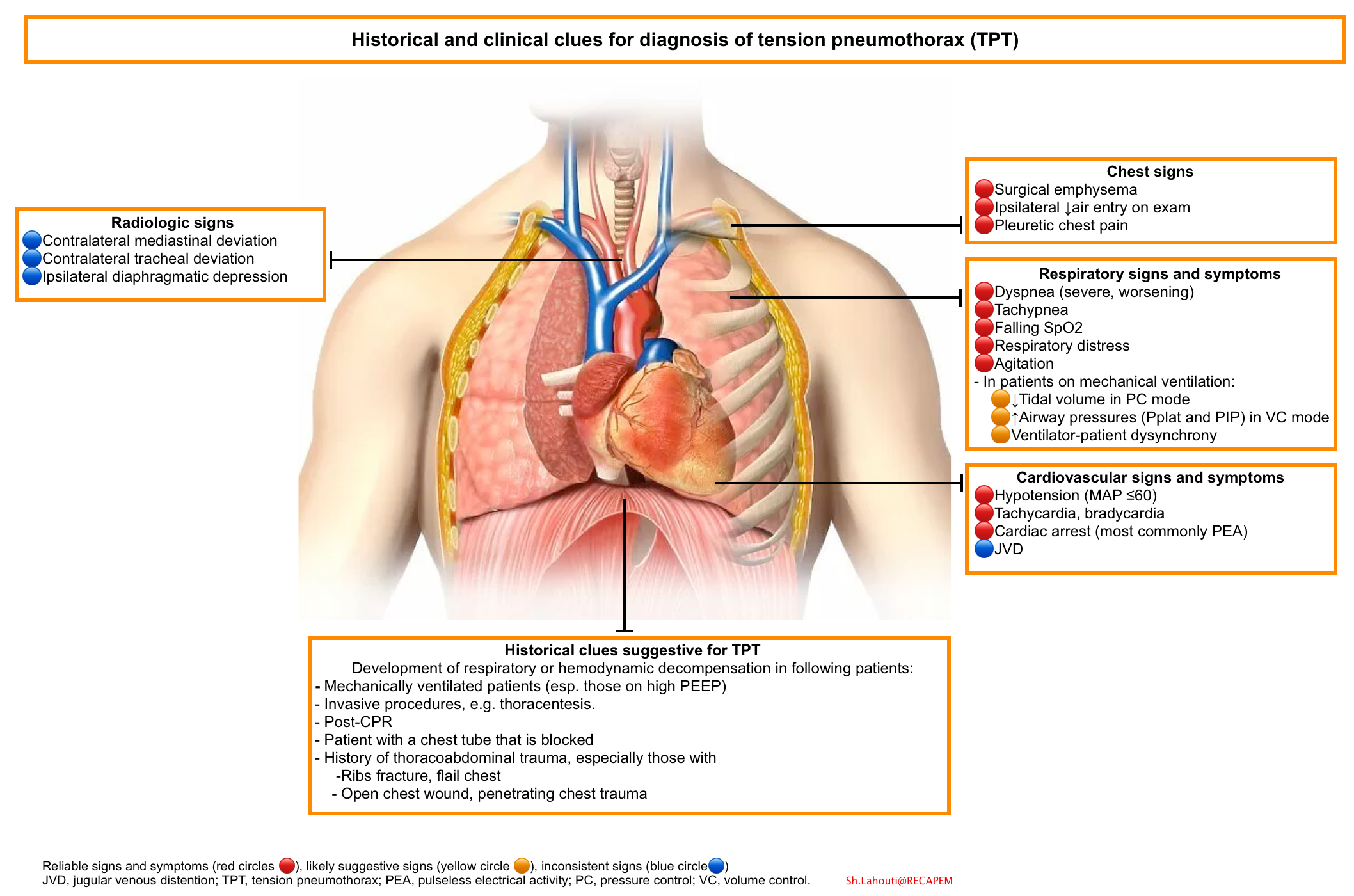
- Traditionally, it has been taught that tension pneumothorax is recognized based on the presence of tracheal deviation away from the involved side, jugular venous distension, profound dyspnea, and hypotension. However, this clinical description is arguably not practical as:
- The classic clinical findings are actually uncommon.
- The clinical presentation of tension pneumothorax depends on the ventilatory status of the patients, as those who are receiving assisted ventilation likely present with sudden hemodynamic and respiratory compromise whereas those breathing unassisted may more often first present with hypoxemia leading to progressive respiratory failure over a more delayed period *.
- In patients who are breathing spontaneously, several compensatory mechanisms likely prevent hemodynamic compromise during progressive pneumothorax volumes, including increasing respiratory rates and tidal volumes and increasingly negative contralateral chest excursions.
- These compensatory mechanisms can maintain arterial blood pressure during tension pneumothorax through:
- Incomplete transmission of pneumothorax-related pressure to the mediastinum and contralateral hemithorax, and
- Maintenance of cardiac blood return through a venous siphon effect from increasingly negative contralateral intrathoracic pressures.
- These compensatory mechanisms can maintain arterial blood pressure during tension pneumothorax through:
- In contrast, patients on positive pressure ventilation are likely incapable of mounting a sufficient compensatory response because of sedation and raised inspiratory pressures.
- Therefore, increased intrapleural pressure throughout the respiratory cycle produces an immediate and marked decrease in cardiac venous return, which often leads to hypotension and may result in cardiac arrest (more on this below).
Epidemiology and causes
From a clinical standpoint, pneumothorax is classified as atraumatic (spontaneous) and traumatic. The two subtypes of atraumatic pneumothorax are primary and secondary.
| Primary spontaneous pneumothorax (PSP) |
Definition
- Referred to a pneumothorax in the absence of trauma and no apparent (clinical) underlying lung disease.
- Classically, PSP is defined in the absence of clinical lung disease such as COPD. However, it is associated with unrecognized underlying lung disease i.e. subpleural blebs.
- On the other hand, further investigations have shown that most patients with apparent PSP may have other more serious underlying lung diseases (e.g. thoracic endometriosis, lymphangioleiomyomatosis).
- Therefore the distinction between PSP and SSP is artificial and both may exist on either end of a continuum *.
Epidemiology
- PSPs occur in people aged 20-30 years, with a peak incidence in the early 20s.
- The age-adjusted incidence of PSP is 7-18 cases per 100,000 persons per year for men and 1.2-6 cases per 100,000 persons per year for women *.
- Risk factors:
- Male sex with an M/F ratio of 6
- Smoking
- Tall thin body habitus
- Genetic predisposition
- Recurrence rate:
- The recurrence rate after the first PSP is ~ 25% (with most of the risk in the first year).
- Risk factors for recurrence *
- Female gender
- Tall stature in men
- Low body weight
- Failure to stop smoking or the presence of respiratory bronchiolitis
- Large initial pneumothorax size *
- Blebs or bulla on chest CT *
- Previous events: The recurrence rate after the second episode of PSP is ~ 60% and up to ~80% after the third recurrence.
Pathogenesis
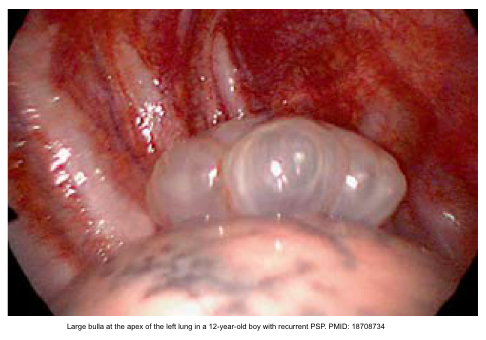
- Subpleural blebs
- PSP typically occurs when small apical subpleural blebs or bullae (i.e. air sacs between the lung tissue and pleura) rupture into the pleural cavity.
| Secondary spontaneous pneumothorax (SSP) |
Definition
- Referred to a pneumothorax that presents as a complication of underlying lung disease.
Epidemiology
- It occurs more frequently in patients aged 60-65 years.
- The general incidence is almost similar to that of PSP *.
- The M/F ratio ~ 3
- Recurrence rates usually are higher as compared to those for PSP, ranging to ~ 50% in patients with COPD and up to 80% in patients with cystic fibrosis
Causes
- Airway disease
- COPD/emphysema, severe asthma, cystic fibrosis *.
- Airway obstruction
- Foreign body aspiration
- Underlying lung disease
- ARDS
- Infection
- TB, necrotizing pneumonia, Pneumocystis jirovecii (carinii)
- Interstitial lung disease
- Idiopathic pulmonary fibrosis, sarcoidosis, etc.
- Connective tissue/inflammatory disease
- Marfan syndrome, Ehlers-Danlos syndrome, hyperhomocysteinemia, alpha-1 antitrypsin, rheumatoid arthritis, polymyositis or dermatomyositis, scleroderma *.
- Malignancy
- Primary lung cancers or metastatic lung disease
- Cystic lung disease (other than emphysema)
- Lymphocytic interstitial pneumonitis (e.g. Sjögren syndrome), Lymphangioleiomyomatosis, pulmonary Langerhans cell histiocytosis
- Miscellaneous
- Anorexia nervosa
- Exercise, illicit drug use, immunosuppressant drugs
- Air travel and scuba diving.
- Pulmonary infarction (due to pulmonary embolism)
| Traumatic pneumothorax |
Definition
- Referred to a pneumothorax that develops in the setting of blunt or penetrating trauma.
- This is the most common cause of pneumothorax.
Causes
- Iatrogenic (most common cause of pneumothorax in ICU)
- Central venous catheterization (44%)
- Thoracentesis (20%)
- Barotrauma due to mechanical ventilation (9%)
- Lung hyperinflation due to over-aggressive bag-mask ventilation may cause pneumothorax.
- Pneumothorax is especially likely if there is right main bronchus intubation.
- Pneumothorax due to mechanical ventilation is more related to the underlying process than the ventilatory setting.
- Most patients with pneumothorax from mechanical ventilation have underlying lung diseases, e.g. obstructive lung disease, and pneumonia.
- Ventilator mode may affect how rapidly the pneumothorax evolves:
- Volume-controlled ventilation will tend to continue to force volume into the pneumothorax, which may cause more aggressive growth and more rapid/explosive development of tension pneumothorax.
- Pressure-controlled ventilation will provide smaller tidal volumes as the pneumothorax grows. As the airway pressure is fixed, the pneumothorax may reach equilibrium with the ventilator (wherein additional gas is not entering the pneumothorax). This may tend to cause the pneumothorax to present in a more gradual/occult fashion.
- The median time from mechanical ventilation to the development of pneumothorax was estimated at 4 days.
- Approximately 10% of patients with first-episode pneumothorax will develop second-episode pneumothorax on the other lung during mechanical ventilation.
- Airway laceration during intubation (e.g. bougie inserted too far).
- Bronchoscopy
- Intercostal nerve block
- Percutaneous or transbronchial lung or mediastinal biopsy
- Surgical procedures involving the thorax, head, and neck e.g. shoulder arthroscopy
- Abdominal procedures
- Tracheostomy
- Non-iatrogenic: Blunt or penetrating trauma, and cardiopulmonary resuscitation.
- Closed pneumothorax
- Open pneumothorax
- When a penetrating traumatic chest wall defect is present, through which atmospheric air enters the pleural space during inspiration (i.e. sucking wound) and exits during expiration.
| Tension pneumothorax |
- The true incidence of TPT is unknown.
- Causes
- TPT is more common in patients with chest trauma and those who are mechanically ventilated.
- Only ~2% of the cases of idiopathic spontaneous pneumothorax may develop TPT.
Clinical presentation and diagnosis
History
- Previous history of pneumothorax (including contralateral side)
- Underlying pulmonary disease associated with pneumothorax, e.g. COPD, CF
- Trauma
- Invasive procedure e.g. CVC insertion, thoracentesis.
- Mechanically ventilated patients.
- Scuba diving.
- Illicit drug use.
Signs and symptoms
- Pneumothoraces can be even further classified as simple, tension. A simple pneumothorax does not have a tension physiology.
| Simple pneumothorax |
- Asymptomatic
- Some patients with mild, chronic pneumothorax may be asymptomatic.
- Dyspnea and chest pain
- The severity of dyspnea can range from mild to severe and relates to the volume of air in the pleural space as well as the degree of pulmonary reserve.
- Dyspnea is profound if the pneumothorax is large, the underlying cardiopulmonary disease is present, or tension pneumothorax develops.
- Chest pain is initially pleuretic. however, later in the course of the disease, the pain may become less pleuritic, more constant, and dull.
- The severity of dyspnea can range from mild to severe and relates to the volume of air in the pleural space as well as the degree of pulmonary reserve.
- Tachycardia
- Signs and symptoms of respiratory distress can be present to variable degrees among the patients.
- Hypoxia and requirement for supplemental oxygen
- Tachypnea
- Use of accessory muscle for respiration
- Absent/decreased breath sound
- In mechanically ventilated patients (more on this, here).
| Tension pneumothorax (TPT) |
- The patient’s appearance is highly variable, ranging from acutely ill with cardiorespiratory compromise to misleadingly healthy appearance.
- The signs and symptoms are not always correlated with the size of the pneumothorax.
- In contrast to traditional teaching, the classic clinical hallmarks of TPT (such as tracheal deviation away from the involved side, profound dyspnea, hypotension, and JVD) are uncommon. In 2015 systemic review *
- Tracheal deviation and hypotension occurred in less than 1 in 5 patients.
- JVD occurred in less than 1 in 20 patients.
- Moreover, the clinical manifestation of tension pneumothorax depends on the ventilatory status of the patients (table below) *.
- In ventilated patients, TPT evolves rapidly with consistent signs of respiratory and cardiac compromise.
- Among mechanically ventilated patients, pneumothorax development is more rapid and explosive among those on volume-controlled rather than pressure-controlled modes of ventilation (discussed above).
- In contrast, awake patients show a greater variability of presentations, which are generally more progressive, with slower decompensation.
- In ventilated patients, TPT evolves rapidly with consistent signs of respiratory and cardiac compromise.

Consistent and reliable findings
- Profound dyspnea
- Tachycardia
- Extreme bradycardia (signifying impending cardiorespiratory arrest)
- Hypotension
- Hypoxia
⚠️Tracheal deviation and neck vein distension should be de-emphasized as classic signs of the disease.
Diagnostic process of tension pneumothorax
- Consider
- Mechanism of pneumothorax and index of suspicion (figure below)
- In mechanically ventilated patients and/or sedated patients
- Early and reliable signs
- Falling SpO2 (immediately)
- Hypotension
- Pre-terminal signs
- Cardiac arrest (PEA most common rhythm )
- Early and reliable signs
- In spontaneously breathing patients
- Early and reliable signs
- Respiratory distress.
- Pre-terminal signs.
- Decreasing respiratory rate and SpO2.
- Hypotension.
- Decreased level of consciousness.
- Early and reliable signs
- Look for other confirmatory signs of TPT
- In mechanically ventilated patients
- Increased ventilation pressure in a volume-cycled mode of ventilation, or decreased tidal volume in those on the pressure-cycled mode of ventilation *.
- Surgical emphysema.
- In spontaneously breathing patients
- Pleuretic chest pain.
- Worsening dyspnea.
- In mechanically ventilated patients
- Lateralize the disease
- Ipsilateral ↓air entry on exam
- Lung US or CXR
- Confirm diagnosis
- Improvement of profound hemodynamic or respiratory compromise following a “decompression alone” (that is, without chest drain placement).
- A continual exit of air throughout the respiratory cycle will add to the diagnostic certainty (unlike a brief hiss during one phase of the respiratory cycle).
- ⚠️Keep in mind that the absence of tracheal deviation or JVD does not rule out the diagnosis of TPT.
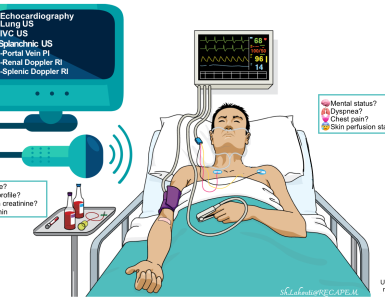
👉In addition to the sonographic features of pneumothorax, the RUSH exam provides other clues for the presence of tension physiology (more on this, below).
Diagnosis of pneumothorax
Background
- Pneumothorax is a radiologic diagnosis.
- The choice of imaging modality is dependent upon the stability of presentation, and the degree of suspicion for competing diagnoses.
- Patients who meet the following criteria are defined as stable *
- RR < 24 bpm
- No dyspnea at rest, speak in full sentences
- 60<HR<120 bpm
- Normal BP for the patient
- Oxygen saturation > 90% RA
- Absence of hemothorax
- Instability typically happens in patients with extensive trauma, tension pneumothorax, or patients with significant underlying lung disease and is characterized by:
- Hemodynamic instability e.g. hypotension, SI>1, extreme tachycardia, confusion
- Severe respiratory distress, e.g. RR >30, accessory use of respiratory muscle, oxygen saturation < 90% while on 60% FiO2, cyanosis.
- Patients who meet the following criteria are defined as stable *
Imaging
CXR
- Diagnostic performance
- The sensitivity of anteroposterior CXR (when compared with CT) is ~40% with a specificity of 99%.
- Finding
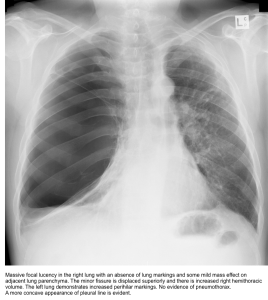
- The classic CXR finding is a thin visceral pleural line lying parallel to the chest wall, separated by a radiolucent band devoid of lung markings.
- Radiologic differential diagnosis
- A large bullae may mimic the radiographic appearance of pneumothorax.
- A clue to differentiating pneumothorax from a giant bulla is that pneumothorax often shows a pleural line that runs parallel to the chest wall, whereas bullae usually have a more concave appearance (figure below).
- Lobar emphysema
- Skin fold artifact
- A large bullae may mimic the radiographic appearance of pneumothorax.
- The size of the pneumothorax can be calculated as:
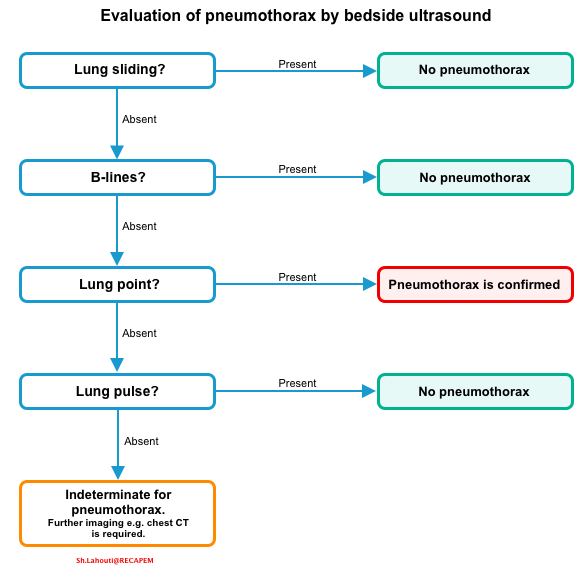
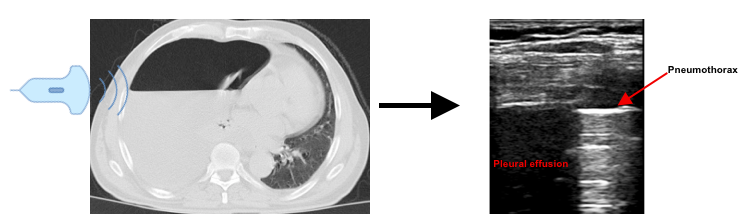
Ultrasound
- Diagnostic performance
- Sensitivity of 98% and specificity of 99%
- Sonographic signs of pneumothorax (media below)
- Absence of lung sliding: Sensitivity 100%, specificity 78%
- The presence of sliding effectively rules out a pneumothorax, however, the absence of lung sliding does not necessarily indicate that a pneumothorax is present.
- Lung sliding is absent in conditions other than pneumothorax, including *
- ARDS, pneumonia with consolidation, and fibrosis (where the visceral pleura cannot move relative to the parietal pleura)
- Contusion
- A non-ventilated lung: Massive atelectasis, main stem intubation, apnea, cardiopulmonary arrest without an airway, stiff lung e.g. severe COPD/asthma
- Pleural effusions
- Absence of B-lines
- Visualization of even one comet-tail essentially rules out the diagnosis of a pneumothorax
- Presence of A-lines
- If lung sliding is absent with the presence of ‘A-lines’, the sensitivity and specificity for pneumothorax is as high as 95 and 94%, respectively.
- Lung-point sign: Sensitivity 79%, specificity 100%
- It occurs at the border of a pneumothorax. More on this here.
- Although the specificity is high, the sensitivity of the ‘lung-point sign’ is relatively low and is not seen in cases of total lung collapse *.
- The location of the lung point helps determine the size of the pneumothorax *.
- A small pneumothorax will rise to the anterior portion of the chest, and therefore the lung point will be located anteriorly.
- As the pneumothorax grows in size, the lung point moves to a progressively more posterior location.
- In the case of complete lung collapse, the lung point may disappear entirely.
- Lung pulsation
- Refers to the rhythmic movement of the pleura in synchrony with the cardiac rhythm.
- The ‘lung pulse’ is a result of cardiac vibrations being transmitted to the lung pleura in poorly aerated lungs.
- The presence of a lung pulse indicates that the lung is fully inflated at the site of probe placement on the chest wall, so there is no pneumothorax at that examination site. The absence of lung pulse indicates the possibility of pneumothorax, as there are other causes for its absence *.
- Absence of lung sliding: Sensitivity 100%, specificity 78%
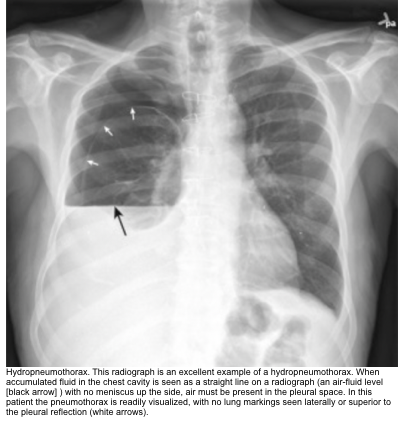
- Sonographic signs of hydropneumothorax
- Hydro-point sign: In ultrasonographic sign of air-fluid level.
- This sign is seen when the ultrasound probe is at the level of the air-fluid interface *.
- The air-fluid interface oscillates up and down due to wavelets in the fluid caused by respiratory or cardiac motion. This causes the image to alternate between showing a pneumothorax and a pleural effusion.
- Hydro-point sign: In ultrasonographic sign of air-fluid level.
- RUSH exam often performed in hemodynamically unstable patients gives helpful clues in identifying the cause(s) of instability *.
- The presence of following features implies the presence of tension physiology *:
- Dilated, fixed IVC
- Dilation (>2.1 cm) and absence of variation with respiration imply a pathologically elevated CVP, consistent with obstructive shock.
- Hyperdynamic right heart with underfilling
- The RV function will be normal or supranormal, with systolic obliteration of the ventricular cavity.
- The RV diameter will be reduced as a result of the reduction in filling/preload.
- Differential diagnosis: Cardiac tamponade
- RV diastolic collapse will be observed in the presence of pericardial effusion.
- Dilated, fixed IVC
- The presence of following features implies the presence of tension physiology *:
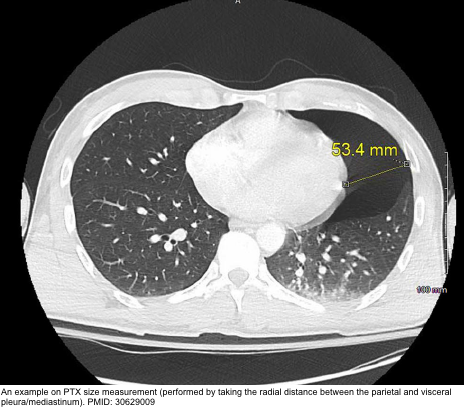
Chest CT
- It is the modality of choice for determining the presence, size, and location of pneumothorax.
- Size: The measurement was performed by taking the radial distance (in millimeters) between the parietal and visceral pleura/mediastinum in a line perpendicular to the chest wall on axial imaging of the largest air pocket * (figure below).
- Small amounts of air in the pleural space and pleural pathology including pleural effusions and adhesions as well as loculations can be better appreciated by CT than chest radiography
- Indications
- Patients who are undergoing chest CT for another indication (e.g. stable patients with trauma undergoing total body CT for additional injuries or patients with suspected pulmonary embolism undergoing CT pulmonary angiography).
- Uncertain diagnosis after CXR (e.g. patients with suspected loculated pneumothorax, complicated bulla, or a complex pleural space).
Differential diagnosis
DDX of simple pneumothorax
- Pleuritis
- Pericarditis (+/- effusion)
- Myocardial ischemia or infarction
- Acute aortic syndrome
- Pneumonia
- Submassive pulmonary embolism
- Musculoskeletal pain
DDx of tension pneumothorax
- Obstructive shock e.g. tamponade, massive PE
- Combined shock
Other diagnostic evaluation
Labs
- Lab tests are not generally helpful for the diagnosis of pneumothorax but may be useful to identify the underlying conditions or to exclude other clinical mimickers
- Complete blood counts
- D-dimer and troponin, only if clinically suspected for PE, AMI
- Alpha-1 antitrypsin level
- HIV serology
- Malignancy screening test
- Serologic testing for suspected Sjögren syndrome
- Homocysteine levels
Diagnostic procedure
- Video-assisted thoracoscopic surgery (VATS), if PSP is a consideration.
- Lung biopsy for suspected interstitial lung disease or malignancy
- Bronchoscopy with bronchoalveolar lavage, when infectious etiology is suspected
General approach to critical patients
- Assess airway, breathing, and circulation (ABC)
- Airway/breathing
- Place the patient on 100% oxygen via a nonrebreather mask
- Immediately perform a needle decompression, or finger thoracostomy, in unstable patients or those with signs of cardiovascular compromise.
- Suspicion of tension pneumothorax based on clinical findings is an indication of immediate pleural decompression.
- Treatment should not be delayed pending a confirmatory ultrasound (if not immediately available) or CXR.
- A tension pneumothorax is confirmed by improvement in vital signs following this step.
- Tube thoracostomy is the definitive treatment and should be performed immediately following needle decompression or finger thoracostomy.
- Suspicion of tension pneumothorax based on clinical findings is an indication of immediate pleural decompression.
- Perform the RUSH exam.
- Close open chest wounds with a 3-sided occlusive dressing (media below).
- In the absence of tension physiology, continue oxygen therapy to maintain an oxygen saturation >90% while awaiting bedside ultrasound (if not performed yet) or Chest CT for a more definitive diagnosis.
- Initial management of pneumothorax is dictated by the severity of the patient’s symptoms and the size of the pneumothorax.
- Once the decision has been made to proceed with evacuation of the pneumothorax, the size of the thoracostomy tube or catheter selected depends upon the likelihood of high-volume air leakage (e.g. large pneumothorax, mechanical ventilation, bronchopleural fistula) or presence of concomitant blood (e.g. large pleural air-fluid level, trauma mechanism).

- ⚠️Avoid the following treatments in patients with pneumothorax:
- High-flow nasal oxygen via nasal cannulae (HFNC)
- Noninvasive ventilation (NIV)
- Chest physical therapy
Initial Therapeutic Options in ED
| Supplemental oxygen |
- Rational
- Supplemental O2 increases the rate of resorption of air from the pleural space by up to six-fold.
- This works by creating a nitrogen gas pressure gradient between the alveolus and trapped air; promoting resorption of air (mostly nitrogen) from the pleural space.
- Oxygen delivery
- 100% humidified oxygen should be delivered at high FiO2 (e.g. via a nonrebreather mask) targeting a SpO2 of 100%
- Avoid high-flow oxygen via nasal cannula (HFNC) since a small amount of positive pressure is delivered to the upper airway and could theoretically worsen the pneumothorax.
- Monitor for hypercapnia in patients with chronic obstructive pulmonary disease.
| Pleural space decompression |
- Indication
- Unstable patients or in whom there is strong clinical suggestion of tension pneumothorax.
- Method
- Needle decompression
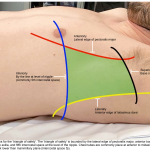
- The preferred approach is the 4th or 5th intercostal space in the anterior to the midaxillary line. This is preferred over the traditional anterior approach (2nd intercostal space in the midclavicular line) *.
- Use a large-bore needle/angiocatheter combination (minimum of 16 gauge).
- After insertion into pleural space, remove the needle, but leave the angiocatheter in place to create a simple pneumothorax.
- Note that this is only a temporary therapeutic maneuver for tension pneumothorax, and a chest tube must also be inserted.
- The preferred approach is the 4th or 5th intercostal space in the anterior to the midaxillary line. This is preferred over the traditional anterior approach (2nd intercostal space in the midclavicular line) *.
- Finger thoracostomy
- If the needle decompression is not effective an open thoracostomy can be started, even without the immediate availability of a chest tube, to help create an exit for the air so that the patient’s respiratory and cardiovascular functions can normalize.
- The preferred approach is the 4th or 5th intercostal space in the anterior to midaxillary line.
- Needle decompression
| Pleural space drainage |
- Method
- Aspiration
- Needle or catheter aspiration (either single or sequential aspirations). See the media below.
- Tube or catheter thoracostomy
- Indications for tube or catheter thoracostomy
- Unstable pneumothorax
- Recurrent pneumothorax
- Pneumothorax in the presence of another indication for drainage such as hemothorax
- Large size (>3cm at apex or alternatively >2cm at hilum)
- Small pneumothoraces that are not improving (or are not stable) over period of observation and oxygenation.
- Indications for tube or catheter thoracostomy
- Aspiration
Initial thoracostomy management
Technique
- Chest tube thoracostomy refers to the insertion of a standard chest tube, while catheter thoracostomy refers to the insertion of a catheter (eg, pigtail catheter)
- Seldinger technique is useful for the placement of smaller-bore thoracostomy catheters (media below).
- Surgical thoracostomy is used for placement of larger diameter tubes (≥16 French). See the media below.
- Insertion site: See triangle of safety here
- Tube positioning
- The chest tube needs to be advanced far enough into the thorax so that its most peripheral intake portal (i.e. the “sentinel hole”) rests within the pleural space.
- Direct the chest tube toward the Apax rather than toward the midline.
- Chest tubes directed medially (i.e., towards the midline) rather than superiorly (i.e., towards the lung apex) are more likely to lean on the mediastinum.
- Selection of chest tube or catheter size
- This is based on the flow rate of air that the device can accommodate *. Large-bore tubes are selected for patients with the following conditions:
- Tension pneumothorax
- Anticipated bigger air leaks, for example, pneumothorax of any size in mechanically ventilated.
- Large pneumothorax
- Recurrent pneumothorax
- Hydropneumothorax (pneumothorax with effusion). Figure below
- Bilateral pneumothorax
- Failed small-bore drainage
- This is based on the flow rate of air that the device can accommodate *. Large-bore tubes are selected for patients with the following conditions:
Confirmation of tube placement
- Look for the presence of tidaling.
- Observe the free flow of blood or fluid.
- Definitive confirmation requires a CXR assessment.
- If the tube and the most proximal hole are not completely within the pleural space, and if the field has remained sterile, advance the tube.
- If the tube is kinked or dysfunctional or the sterile field has been lost and advancement is required, place a new tube in a sterile fashion through the same tract.
- If the tube has been advanced too far, simply withdraw it to the correct depth.
Securing the tube
- Once the position of the tube has been verified with a radiograph, secure it.
- Use a large 0 or 1-0 silk sutures.
- Technique
- Stay suture, in which the same suture that closes the skin incision is used to hold the tube (media below).
- After this suture is used to close the skin incision at the site of insertion of the tube, wrap the ends tightly and repeatedly around the chest tube, and tie it securely. Tie the sutures tightly enough to indent the chest tube slightly and avoid slippage.
- If the skin incision is especially long, use additional simple sutures to close it completely.
- Horizontal mattress suture approximately 1 cm across the incision on either side of the tube, essentially encircling it (media below).
- Secure it with a simple knot that can easily be untied so that it can be opened and retied to close the incision after the tube has been removed
- Stay suture, in which the same suture that closes the skin incision is used to hold the tube (media below).
- Apply an occlusive dressing of petrolatum-impregnated gauze at the point where the tube enters the skin to help reduce air leaks.
- Cover the skin with two or more gauze pads with a Y -shaped cut from the middle of one side to the center.
- Secure this dressing with a wide (8 cm to 9 cm) cloth or elastic adhesive tape.
- All the connections including the connection between the chest tube and with pleural vac tube should also be taped.
Setting up drainage and suction system
- How to set up drainage and suction systems? 👉See media below.
- Suction
- For the majority of patients, suction is not initially applied and the tube or catheter is connected to a water seal device only*.
- Indications
- Failure of lung re-expansion within the next 24-48h
- Worsening pneumothorax despite chest tube drainage
- Persistent air leak
- Set up
- Wall suction, starting with low rates of -10 cm H2O and increasing to -20 cm H2O using a high-pressure-low volume system.
- Basic definitions
- Tidaling: With a chest tube in the pleural space, the water level should fluctuate in the water seal chamber. This is known as tidaling, and should correspond with respiration.
- Tidaling is more apparent when the suction is off. When suction is on, the amount of tidaling will potentially decrease.
- Air leak: Is seen as bubbling in the water seal chamber (more on this, here).
- Classifying air leak and corresponding etiology *
- Forced expiratory air leak: only noted with coughing or Valsalva
- Expiratory air leak: alveolar-pleural fistulas
- Inspiratory air leak: ventilated patient, bronchopleural fistula, alveolar-pleural fistula
- Continuous air leak: ventilated patient, true bronchopleural fistula
- Classifying air leak and corresponding etiology *
- Tidaling: With a chest tube in the pleural space, the water level should fluctuate in the water seal chamber. This is known as tidaling, and should correspond with respiration.
Prophylactic antibiotic
- Despite the absence of specific standards, it appears reasonable to provide short-term antibiotic prophylaxis (first-generation cephalosporins during the first 24 hours) for tube thoracostomy performed in the ED.
Follow-up thoracostomy management
Complications of chest drain insertion 👉See appendix
- Re-expansion pulmonary edema (RPE)
- The incidence ranges between 1‑14%, with a mortality rate as high as 20% *.
- It usually occurs on the side ipsilateral to the reexpanded lung (unilaterally). Rarely it can occur bilaterally or contralaterally *.
- Pathophysiology: Increased endothelial permeability mediated by oxygen free radicals and multiple inflammatory mediators
- Clinical features
- Onset: The symptoms of RPE usually appear within the first 2 hours following pulmonary reexpansion, but may be delayed by as many as 24‑48 h *.
- Presentation: Can range from an asymptomatic radiographic finding to cardio‑respiratory collapse and shock.
- RPE usually lasts clinically for as long as 1‑2 days, but may take anywhere from 5 to 7 days to resolve *.
- Risk factors *
- Younger age (<40)
- Longer duration of lung collapse (>4 days)
- Large pneumothorax (>30% of a single lung)
- Concurrent presence of a pleural effusion *
- Rapid re-expansion
- Excessive suction
- Preventive measures should be employed for those patients at high risk for RPE including
- Using a smaller chest tube diameter.
- Use of a water seal instead of suction.
- Treatment: Is supportive
- Hemodynamic support (e.g. vasopressors)
- Discontinue suction
- Positioning: In unilateral RPE, positioning the patient in a lateral decubitus position with the affected side up will reduce intrapulmonary shunting and improve oxygenation *.
- If clinical deterioration continues, asynchronous differential lung ventilation may be beneficial *.
- Recurrent pneumothorax after chest tube removal
- Incidence: 4%-8% of cases
- Etiology *
- Premature tube removal (i.e. before full lung re‑expansion)
- An occult air leak
- Air entering the pleural space during removal (this is especially common in patients with relatively thin chest wall anatomy *).
- Management
- Observation with supplemental oxygenation: For patients with small, asymptomatic pneumothorax.
- Insertion of a new thoracostomy tube: Patients with symptomatic or large pneumothorax
- Prevention
- Proper technique of chest tube removal (more on this below).
Daily bedside assessment
- Daily assessment of patients within the first 1-5 days should be performed, and include evaluation for
- Symptoms
- The presence of an air leak
- Complications of the catheter or chest tube (e.g. blockage, pain, bleeding)
- CXR
Common problems (media below)
- Absent tidaling. Possible causes include:
- Lung fully expanded
- Chest tube not in pleural space (air leak would be present)
- Chest tube blocked (kinked, obstruction)
- High level of water in the tidaling chamber
- Air leak
- In pneumothorax, an air leak is normal initially (any time that air is evacuating out of the pleural space, an air leak should be seen).
- Troubleshooting/evaluation
- Increased and continuous air leak
- Check if the chest tube is outside the pleura, and check the drainage tube and system.
- Persistent air leak (continues for > ~5 days)
- It could be a sign of bronchopleural fistula.
- In this condition, evaluate for the following possible causes (in order of sequence):
- Check whether the leak is coming from around the chest tube at the skin entry site, or from the drainage tube or drainage chamber.
- This is classically done by clamping the tube (for ~30 sec) at different locations to isolate the site of the leak.
- If the air leak is not coming from the tube and drainage system, the primary problem is the lung.
- Perform chest CT to evaluate for lung re-expansion.
- These patients require a more aggressive approach for defect closure since the longer an air leak persists, the less likely it becomes that the leak will close spontaneously and the more likely that a definitive intervention (eg, blebectomy and pleurodesis) will be required.
- Check whether the leak is coming from around the chest tube at the skin entry site, or from the drainage tube or drainage chamber.
- Increased and continuous air leak
Removal of chest tube: Assessment
- Assessment
- Get a CXR to confirm lung has fully expanded.
- Confirm that visible air leak is absent and air does not accumulate when suction is removed.
- Daily fluid output (<100-300 mL)
- If the lung fully expanded with a sealed air leak
- Clamp the chest tube/catheter for an additional 4 to 12 hours. Clamping the chest prevents inapparent drainage of small amounts of air through the water seal and thus allows recognition of small leaks that would otherwise be missed.
- Absence of pneumothorax: Remove the chest tube.
- Recurrence of pneumothorax: Unclamped and repeat the process. Continue with tube or catheter drainage to water seal for another 24 to 48 hours.
- Clamp the chest tube/catheter for an additional 4 to 12 hours. Clamping the chest prevents inapparent drainage of small amounts of air through the water seal and thus allows recognition of small leaks that would otherwise be missed.
- If the lung is not fully expanded but the air leak is sealed
- Possible causes include
- Chest tube blockage: Flush the tube/catheter
- Chest tube malposition: Perform chest CT
- Pneumothorax ex vacuo
- This is an uncommon complication of lobar lung collapse.
- It is described as the result of gas being drawn into the pleural space due to acute endobronchial obstruction with lobar collapse that is fully reversible once the obstruction is resolved *.
- The pneumothorax spontaneously resolves when the bronchial obstruction is relieved and the lobe re-expands. The noncompliant lung is usually unresponsive to chest drain insertion so it should not be used in asymptomatic patients unless there is a concern for a trapped lung.
- Possible causes include
Removal of chest tube: Technique
- If the removal criteria above are met, prepare for the removal of the chest tube.
- Eliminate suction before removal.
- Be prepared for close monitoring of the patient after removal (the patient may develop respiratory distress after removal due to recurrent pneumothorax).
- See the media below.
Special conditions
Tension pneumothorax
- Tension pneumothorax is a medical emergency. Diagnosis should often be made clinically in critically ill patients.
- Do not delay intervention (e.g. waiting for chest US, if not readily available), If clinical suspicion for TPT is high.
- In unstable patients, with impending respiratory or hemodynamic crash, immediately perform needle decompression or finger thoracostomy followed by tube thoracostomy.
Traumatic pneumothorax
Management
- Pleural drainage. Indications include
- Respiratory distress, hypoxia, or hemodynamic instability; or
- Anticipated prolonged transport time or transport by air ambulance; or
- Increased size of pneumothorax on serial imaging; or
- Pneumothorax size > 35mm on chest CT *
- Hemopneumothorax > 300 mL
- Observation
- Pneumothorax size < 35mm on chest CT can be safely observed.
Occult pneumothorax
- Referred to a pneumothorax which is not visible on a plain CXR but seen on chest CT.
- Management
- Close observation is safe in blunt chest trauma if the following conditions are met *
- Occult pneumothorax < 8mm on CT, and
- Asymptomatic and spontaneously breathing patients *
- Close observation can also be considered as an option in patients with occult pneumothorax who are being ventilated mechanically if *
- MV is planned for < 4-5 days
- Absence of multiple-trauma
- No significant traumatic brain injury
- Good cardiovascular or respiratory reserve
- Close observation is safe in blunt chest trauma if the following conditions are met *
Primary spontaneous pneumothorax (PSP)
Clinically stable patient with small PSP
- Observe in the ED for 3 to 6 hours and be discharged home if a repeated CXR excludes progression of the PSP *.
- Patients should be provided with careful instructions for follow-up within 12 hours to 2 days.
- Patients may be admitted for observation if they live distant from emergency services or if follow-up care is considered unreliable.
- Aspiration or thoracostomy may be required in patients
- Recurrent (second episode) PSP
- If PSP enlarges on repeat CXR *
Clinically stable patients with large PSP
- Chest tube or catheter thoracostomy is indicated in most patients *.
- Observation
- A conservative approach such as observation has been shown to be equivalent to aspiration or chest tube drainage in patients with large PSP *.
- Observation should only be considered as an option in otherwise healthy patients who have mild symptoms, no hemodynamic compromise, no oxygen requirement, and who can ambulate comfortably.
Recurrent PSP
- A chest tube or catheter thoracostomy should be placed for most patients.
- Most patients with recurrent PSP require definitive therapy (e.g. pleurodesis) preferably during hospitalization.
Secondary spontaneous pneumothorax
General supportive measures and considerations
- Supplemental oxygenation
- Treat the underlying lung disease
- For example, pneumothorax may precipitate or be a complication of a chronic obstructive pulmonary disease (COPD) exacerbation or asthma attack, necessitating therapy with nebulized bronchodilators and corticosteroids.
- Admit the patient
- Almost all patients with SSP should be hospitalized because the underlying lung disease increases the risk for an adverse outcome (e.g. respiratory failure, cardiovascular collapse, recurrent event) *.
- Consider definitive treatment
- Most patients with SSP should have a definitive intervention (e.g. pleurodesis) after their first event to prevent recurrence.
Stable patients with SSP
- Most patients with an SSP should be treated with a catheter or chest tube thoracostomy.
Unstable patients with SSP
- Instability due to pneumothorax (including tension pneumothorax) is more common in patients with SSP than primary spontaneous pneumothorax (PSP).
- Patients who are unstable due to SSP should undergo chest tube thoracostomy or alternatively, needle decompression of the pleural space, if chest tube decompression is delayed.
RECAP
- If tension pneumothorax is highly suspicious based on clinical findings (e.g. mechanism of injury, cardiorespiratory compromise), immediate pleural decompression should be performed and not delayed for radiologic confirmation of tension pneumothorax.
- Improvement of profound hemodynamic or respiratory compromise following a “decompression alone” confirms the diagnosis of tension pneumothorax.
- The absence of tracheal deviation and JVD does not exclude the diagnosis of tension pneumothorax.
- Avoid the following treatments in patients with pneumothorax:
- High-flow nasal oxygen via nasal cannulae (HFNC)
- Noninvasive ventilation (NIV)
- Chest physical therapy
- In the presence of increasing, continuous, or persistent air leaks; first, check the drainage tube and system for disconnection/malfunction.
- Closely monitor the patient after tube removal, since respiratory distress may happen secondary to recurrence of pneumothorax.
Appendix
Complication of chest drain insertion
Media
Pigtail Insertion for Pneumothorax
Surgical placement of large tubes
Securing a chest tube: Stay suture
Securing a chest tube: Horizontal mattress suture
Setting up drainage and suction system
Basic of chest tube management
References
1. PMID: 34527359. Thachuthara-George J. Pneumothorax in patients with respiratory failure in ICU. J Thorac Dis. 2021 Aug;13(8):5195-5204. doi: 10.21037/jtd-19-3752.
2. PMID: 15611534. Leigh-Smith S, Harris T. Tension pneumothorax–time for a re-think? Emerg Med J. 2005 Jan;22(1):8-16. doi: 10.1136/emj.2003.010421.
3. PMID: 26170077. Bintcliffe OJ, Hallifax RJ, Edey A, Feller-Kopman D, Lee YC, Marquette CH, Tschopp JM, West D, Rahman NM, Maskell NA. Spontaneous pneumothorax: time to rethink management? Lancet Respir Med. 2015 Jul;3(7):578-88. doi: 10.1016/S2213-2600(15)00220-9.
4. PMID: 517861. Melton LJ 3rd, Hepper NG, Offord KP. Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. Am Rev Respir Dis. 1979 Dec;120(6):1379-82. doi: 10.1164/arrd.1979.120.6.1379.
5. PMID: 30002105. Walker SP, Bibby AC, Halford P, Stadon L, White P, Maskell NA. Recurrence rates in primary spontaneous pneumothorax: a systematic review and meta-analysis. Eur Respir J. 2018 Sep 6;52(3):1800864. doi: 10.1183/13993003.00864-2018.
6. PMID: 29290080. Hofmann HS, Suttner T, Neu R, Potzger T, Szöke T, Grosser C, Ried M. Burden between Undersupply and Overtreatment in the Care of Primary Spontaneous Pneumothorax. Thorac Cardiovasc Surg. 2018 Oct;66(7):575-582. doi: 10.1055/s-0037-1609011. Epub 2017 Dec 31.
7. PMID: 22785214. Casali C, Stefani A, Ligabue G, Natali P, Aramini B, Torricelli P, Morandi U. Role of blebs and bullae detected by high-resolution computed tomography and recurrent spontaneous pneumothorax. Ann Thorac Surg. 2013 Jan;95(1):249-55. doi: 10.1016/j.athoracsur.2012.05.073. Epub 2012 Jul 10.
8. PMID: 10899243. Gupta D, Hansell A, Nichols T, Duong T, Ayres JG, Strachan D. Epidemiology of pneumothorax in England. Thorax. 2000 Aug;55(8):666-71. doi: 10.1136/thorax.55.8.666.
9. PMID: 18708734. Noppen M, De Keukeleire T. Pneumothorax. Respiration. 2008;76(2):121-7. doi: 10.1159/000135932. Epub 2008 Jun 26.
10. PMID: 10727592. Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med. 2000 Mar 23;342(12):868-74. doi: 10.1056/NEJM200003233421207.
11. PMID: 25563887. Roberts DJ, Leigh-Smith S, Faris PD, Blackmore C, Ball CG, Robertson HL, Dixon E, James MT, Kirkpatrick AW, Kortbeek JB, Stelfox HT. Clinical Presentation of Patients With Tension Pneumothorax: A Systematic Review. Ann Surg. 2015 Jun;261(6):1068-78. doi: 10.1097/SLA.0000000000001073.
12. PMID: 11171742. Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, Luketich JD, Panacek EA, Sahn SA; AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001 Feb;119(2):590-602. doi: 10.1378/chest.119.2.590.
13. PMID: 20696690. MacDuff A, Arnold A, Harvey J; BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010 Aug;65 Suppl 2:ii18-31. doi: 10.1136/thx.2010.136986.
14. PMID: 15942336. Lichtenstein DA, Mezière G, Lascols N, Biderman P, Courret JP, Gepner A, Goldstein I, Tenoudji-Cohen M. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005 Jun;33(6):1231-8. doi: 10.1097/01.ccm.0000164542.86954.b4.
15. PMID: 22416161. Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012 Jan;5(1):76-81. doi: 10.4103/0974-2700.93116.
16. PMID: 25056671. Volpicelli G, Boero E, Sverzellati N, Cardinale L, Busso M, Boccuzzi F, Tullio M, Lamorte A, Stefanone V, Ferrari G, Veltri A, Frascisco MF. Semi-quantification of pneumothorax volume by lung ultrasound. Intensive Care Med. 2014 Oct;40(10):1460-7. doi: 10.1007/s00134-014-3402-9. Epub 2014 Jul 24.
17. PMID: 23397048. De Luca C, Valentino M, Rimondi MR, Branchini M, Baleni MC, Barozzi L. Use of chest sonography in acute-care radiology(). J Ultrasound. 2008 Dec;11(4):125-34. doi: 10.1016/j.jus.2008.09.006. Epub 2008 Nov 6.
18. PMID: 24355346. Volpicelli G, Boero E, Stefanone V, Storti E. Unusual new signs of pneumothorax at lung ultrasound. Crit Ultrasound J. 2013 Dec 19;5(1):10. doi: 10.1186/2036-7902-5-10.
19. PMID: 19945597. Perera P, Mailhot T, Riley D, Mandavia D. The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically lll. Emerg Med Clin North Am. 2010 Feb;28(1):29-56, vii. doi: 10.1016/j.emc.2009.09.010.
20. PMID: 28960428. Lanks CW, Correa V. Advantages of Cardiopulmonary Ultrasound in Post-Cardiopulmonary Resuscitation Tension Pneumothorax. J Ultrasound Med. 2018 Apr;37(4):819-822. doi: 10.1002/jum.14437. Epub 2017 Sep 29.
21. PMID: 30629009. Bou Zein Eddine S, Boyle KA, Dodgion CM, Davis CS, Webb TP, Juern JS, Milia DJ, Carver TW, Beckman MA, Codner PA, Trevino C, de Moya MA. Observing pneumothoraces: The 35-millimeter rule is safe for both blunt and penetrating chest trauma. J Trauma Acute Care Surg. 2019 Apr;86(4):557-564. doi: 10.1097/TA.0000000000002192.
22. PMID: 29372629. Porcel JM. Chest Tube Drainage of the Pleural Space: A Concise Review for Pulmonologists. Tuberc Respir Dis (Seoul). 2018 Apr;81(2):106-115. doi: 10.4046/trd.2017.0107. Epub 2018 Jan 24.
23. PMID: 20696690. MacDuff A, Arnold A, Harvey J; BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010 Aug;65 Suppl 2:ii18-31. doi: 10.1136/thx.2010.136986.
24. PMID: 12469484. Cerfolio RJ. Chest tube management after pulmonary resection. Chest Surg Clin N Am. 2002 Aug;12(3):507-27. doi: 10.1016/s1052-3359(02)00015-7.
25. PMID: 25024942. Kwiatt M, Tarbox A, Seamon MJ, Swaroop M, Cipolla J, Allen C, Hallenbeck S, Davido HT, Lindsey DE, Doraiswamy VA, Galwankar S, Tulman D, Latchana N, Papadimos TJ, Cook CH, Stawicki SP. Thoracostomy tubes: A comprehensive review of complications and related topics. Int J Crit Illn Inj Sci. 2014 Apr;4(2):143-55. doi: 10.4103/2229-5151.134182.
26. PMID: 26016583. Mao M, Hughes R, Papadimos TJ, Stawicki SP. Complications of chest tubes: a focused clinical synopsis. Curr Opin Pulm Med. 2015 Jul;21(4):376-86. doi: 10.1097/MCP.0000000000000169.
27. PMID: 22028963. Kesieme EB, Dongo A, Ezemba N, Irekpita E, Jebbin N, Kesieme C. Tube thoracostomy: complications and its management. Pulm Med. 2012;2012:256878. doi: 10.1155/2012/256878. Epub 2011 Oct 16.
28. PMID: 22472408. Anand RJ, Whelan JF, Ferrada P, Duane TM, Malhotra AK, Aboutanos MB, Ivatury RR. Thin chest wall is an independent risk factor for the development of pneumothorax after chest tube removal. Am Surg. 2012 Apr;78(4):478-80.
29. PMID: 23244504. Kim YS, Susanto I, Lazar CA, Zarrinpar A, Eshaghian P, Smith MI, Busuttil R, Wang TS. Pneumothorax ex-vacuo or “trapped lung” in the setting of hepatic hydrothorax. BMC Pulm Med. 2012 Dec 17;12:78. doi: 10.1186/1471-2466-12-78.
30. PMID: 30629009. Bou Zein Eddine S, Boyle KA, Dodgion CM, Davis CS, Webb TP, Juern JS, Milia DJ, Carver TW, Beckman MA, Codner PA, Trevino C, de Moya MA. Observing pneumothoraces: The 35-millimeter rule is safe for both blunt and penetrating chest trauma. J Trauma Acute Care Surg. 2019 Apr;86(4):557-564. doi: 10.1097/TA.0000000000002192.
31. PMID: 21610419. Moore FO, Goslar PW, Coimbra R, Velmahos G, Brown CV, Coopwood TB Jr, Lottenberg L, Phelan HA, Bruns BR, Sherck JP, Norwood SH, Barnes SL, Matthews MR, Hoff WS, de Moya MA, Bansal V, Hu CK, Karmy-Jones RC, Vinces F, Pembaur K, Notrica DM, Haan JM. Blunt traumatic occult pneumothorax: is observation safe?–results of a prospective, AAST multicenter study. J Trauma. 2011 May;70(5):1019-23; discussion 1023-5. doi: 10.1097/TA.0b013e318213f727.
32. PMID: 21307755. Mowery NT, Gunter OL, Collier BR, Diaz JJ Jr, Haut E, Hildreth A, Holevar M, Mayberry J, Streib E. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011 Feb;70(2):510-8. doi: 10.1097/TA.0b013e31820b5c31.
33. PMID: 31995686. Brown SGA, Ball EL, Perrin K, Asha SE, Braithwaite I, Egerton-Warburton D, Jones PG, Keijzers G, Kinnear FB, Kwan BCH, Lam KV, Lee YCG, Nowitz M, Read CA, Simpson G, Smith JA, Summers QA, Weatherall M, Beasley R; PSP Investigators. Conservative versus Interventional Treatment for Spontaneous Pneumothorax. N Engl J Med. 2020 Jan 30;382(5):405-415. doi: 10.1056/NEJMoa1910775.
34. PMID: 16946095. Tschopp JM, Rami-Porta R, Noppen M, Astoul P. Management of spontaneous pneumothorax: state of the art. Eur Respir J. 2006 Sep;28(3):637-50. doi: 10.1183/09031936.06.00014206.




Add comment