24 May 2025, by Abdolghader Pakniyat, peer reviewed by Dr. Shahriar Lahouti
Why Choose VBG Over ABG?
- VBG is easier to obtain, less painful, and faster than arterial sampling. In addition, it significantly reduces the risk of complications. Because it uses venous access, it avoids the hazards associated with arterial puncture, making it an appealing choice in many ED scenarios.
- However, VBG isn’t a one-to-one substitute for ABG in all cases.
- Use your judgment—there are clear situations where ABG is still king.
How to Interpret a VBG: Parameter by Parameter
1. pH of a VBG
- Correlates well with ABG pH.
- Mean difference: 0.033–0.035
- VBG pH is reliable for:
- Diabetic ketoacidosis (DKA)
- COPD exacerbations
- ⚠️ Be cautious in:
- Mixed acid-base disorders
- Hypotension
- Cardiac arrest
💡Takeaway: pH is usually okay—unless the patient is crashing or complex.
2. pCO₂ of a VBG
- NOT reliable to match ABG pCO₂, especially in hypercapnia.
- BUT⤵️
- If VBG pCO₂ < 45 mmHg ➡️ 100% NPV for ABG pCO₂ < 50.
- ✅ Good for ruling out hypercapnia.
- ❌ If > 45 mmHg, get an ABG to confirm.
💡Takeaway: Use VBG pCO₂ to exclude hypercapnia, not confirm it.
3. HCO₃⁻ of a VBG
- Correlates reasonably well with ABG bicarbonate.
- Difference: ~1.03 to 1.41
- Caution in COPD: discrepancy could be as large as ±10 mmol/L.
💡Takeaway: Works in most, but not reliable in COPD or hypercapnic patients.
4. Lactate in a VBG
- Venous lactate correlates well with ABG only if <2 mmol/L.
- In trauma or shock, VBG lactate may be underestimated.
💡Takeaway: Trust VBG lactate only when it’s low (<2). Otherwise, go ABG.
PEARLS TO REMEMBER
🔸 VBG = ✅ for pH and HCO₃⁻, unless hypotensive or mixed disorder.
🔸 VBG = ❌ for accurate pCO₂ if >45 mmHg.
🔸 VBG = ✅ to rule out hypercapnia.
🔸 VBG lactate = ✅ if <2; ❌ if trauma/shock.
🔸 If the patient’s crashing or complex, get the ABG.
Bedside Rule of Thumb
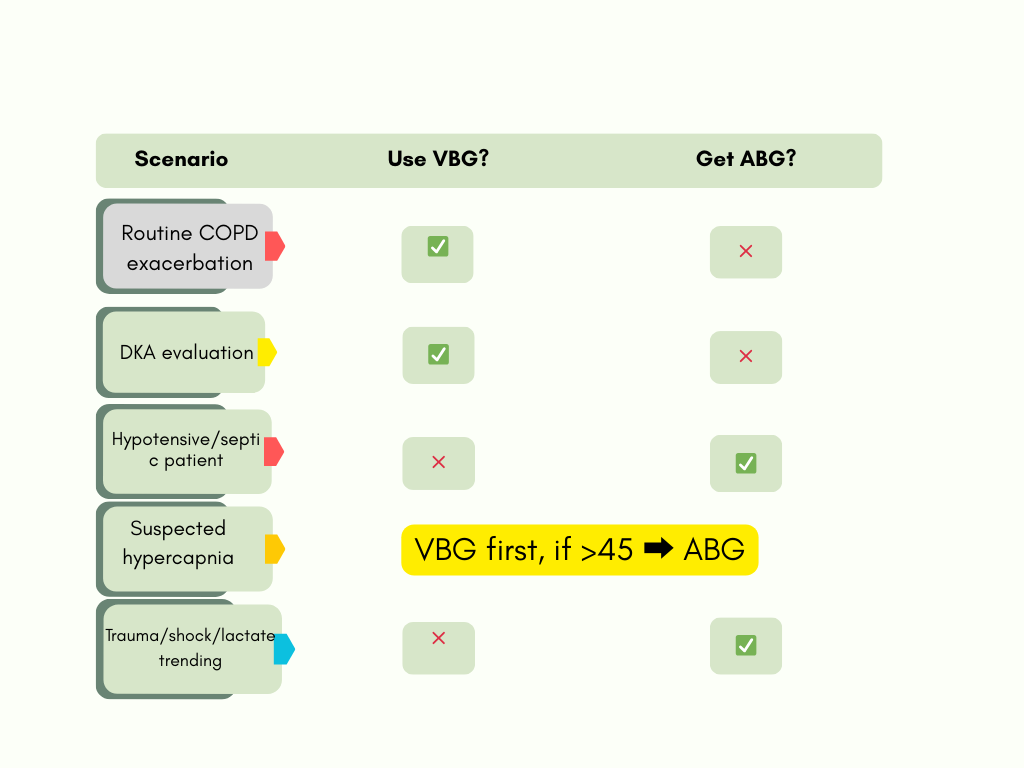
🚨 WHEN TO CHECK BLOOD GAS IN THE ED: CLINICAL SCENARIOS
1. Suspected Acid-Base Disturbance
- DKA: Evaluate metabolic acidosis and guide insulin/fluid therapy.
- Metabolic acidosis / Uremia in ESRD patients.
- Toxic ingestions (e.g., Methanol, Ethylene glycol, Salicylates).
- ✅ VBG is usually fine — unless hypotensive or altered.
2. Suspected Hypercapnia
- COPD exacerbation: Watch for CO₂ narcosis.
- OSA or obesity hypoventilation: Daytime hypercapnia.
- Sedative/ Opioid intoxication: Risk of hypoventilation.
- VBG to rule out if pCO₂ <45
- ABG if >45 or if the patient is obtunded.
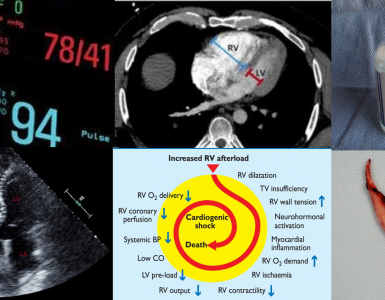
3. Shock / Cardiac Arrest
- Shock Hypovolemic or Cardiogenic shock: Tissue hypoxia, acidosis.
- Post-arrest: pH and CO₂ can guide post-ROSC management.
- Always ABG — venous values are unreliable due to poor perfusion.
4. Lactic Acidosis
- Sepsis: Lactate trending “may” be used for perfusion monitoring. Read more on this 👉 here.
- Seizures or strenuous exertion: Lactate spikes briefly. More on lactate👉 here.
- VBG if < 2
- ABG if lactate is expected to be high or the patient is in shock.
5. Tox / Overdose
- Salicylates: Combined respiratory alkalosis + metabolic acidosis.
- TCA: Acidosis worsens toxicity — pH >7.45 target.
- VBG for trending.
- ABG when you need exact pCO₂ and acid-base precision.
6. Respiratory Failure / Intubation Planning
- Status asthmaticus: Track CO₂ retention.
- ARDS or pneumonia: Oxygenation/vent settings.
- VBG pre-intubation to trend.
- ABG post-intubation or in ARDS, where precise CO₂/O₂ data matters.
Emergency Medicine Wisdom
“If your patient is stable and you just need acid-base direction—go VBG.
If your patient is crashing—go ABG. Don’t gamble on correlation when it matters most.”
Going Further
- Converting VBG to ABG (Josh Farkas-PulmCrit)
- Answers to ABG/VBG questions (Josh Farkas-PulmCrit)
- Approaching undifferentiated cardiopulmonary failure: Which tests are most useful? (PulmCrit)
- pH-Guided Fluid Resuscitation (Josh-Farkas- PulmCrit)
Key References
- Zeserson E, et al. Correlation of venous blood gas and pulse oximetry with arterial blood gas in the undifferentiated critically ill patient. J Intensive Care Med. 2018;33(3):176–181.
- Bloom BM. The role of venous blood gas in the emergency department: a systematic review and meta-analysis. Eur J Emerg Med. 2014;21(2):81–88.
- Kelly A-M. Validation of venous pCO₂ to screen for arterial hypercarbia in patients with chronic obstructive airway disease. J Emerg Med. 2005;28(4):377–379.
- Byrne AL, et al. Peripheral venous and arterial blood gas analysis in adults: are they comparable? A systematic review and meta-analysis. Respirology. 2014;19(2):168–175.



Add comment