29 November, 2020 by Shahriar Lahouti. Last update 8 February 2023.

CONTENTS
- Preface
- Definition
- Pathophysiology
- Etiology
- Evaluation of syncope in ED
- Diagnosis
- Risk stratification
- Management & Disposition
- Specific condition
- Going further
- References
Preface
Syncope accounts for common ED visits and hospital admission. Although most common causes of syncope are benign, identification of life threatening causes associated with syncope is sometimes challenging 1,2. Recent studies and multiple guidelines have clarified the definition and pathophysiology of syncope which was confusing in the past. In the following discussion adult syncope is revisited in the light of these guidelines.
ACS, acute coronary syndrome
AF, atrial fibrillation
AMI, acute myocardial infarction
AS, aortic stenosis
AVB, atrioventricular block
BBB, bundle branch block
CM, cardiomyopathy
DCM; dilated cardiomyopathy
FND, focal neurologic deficit
HCM, hypertrophic cardiomyopathy
HF, heart failure
IHD, ischemic heart disease
IVCD, intraventricular conduction disturbance
LBBB, left bundle branch block
LOC, loss of consciousness
LVH, left ventricular hypertrophy
LQTS, long QT syndrome
LVEF, left ventricle ejection fraction
MI, myocardial infarction
MS, mitral stenosis
OH, orthostatic hypotension
SVT, supraventricular tachycardia
TIA, transient ischemic attack
TLOC, transient loss of consciousness
PE, pulmonary embolism
PH, pulmonary hypertension
PMVT, polymorphic ventricular tachycardia
PPS, psychogenic pseudosyncope
SAH, subarachnoid hemorrhage
SCD, sudden cardiac death
SND, sinus node dysfunction
VT, ventricular tachycardia
VVS, vasovagal syncope
WPW, Wolff-Parkinson-White syndrome
Definition
Syncope is defined as a symptom that present with an abrupt “transient loss of consciousness” associated with inability to maintain postural tone, with rapid and spontaneous recovery and return to baseline neurologic function within seconds 3 4. There should not be clinical features of other non-syncope causes of loss of consciousness, such as seizure, antecedent head trauma, or apparent LOC (ie, pseudosyncope)
Relevant terms and definitions
- TLOC
- It is defined as a state of real or apparent LOC with loss of awareness, characterized by amnesia for the period of unconsciousness, abnormal motor control, loss of responsiveness, and a short duration (self-limited).
- Presyncope
- The symptoms before syncope. These symptoms could include extreme lightheadedness; visual sensations, such as “tunnel vision” or “graying out”; and variable degrees of altered consciousness without complete loss of consciousness. Presyncope could progress to syncope, or it could abort without syncope.
- Psychogenic pseudosyncope
- A syndrome of apparent but not true loss of consciousness that may occur in the absence of identifiable cardiac, reflex, neurological, or metabolic causes
Pathophysiology
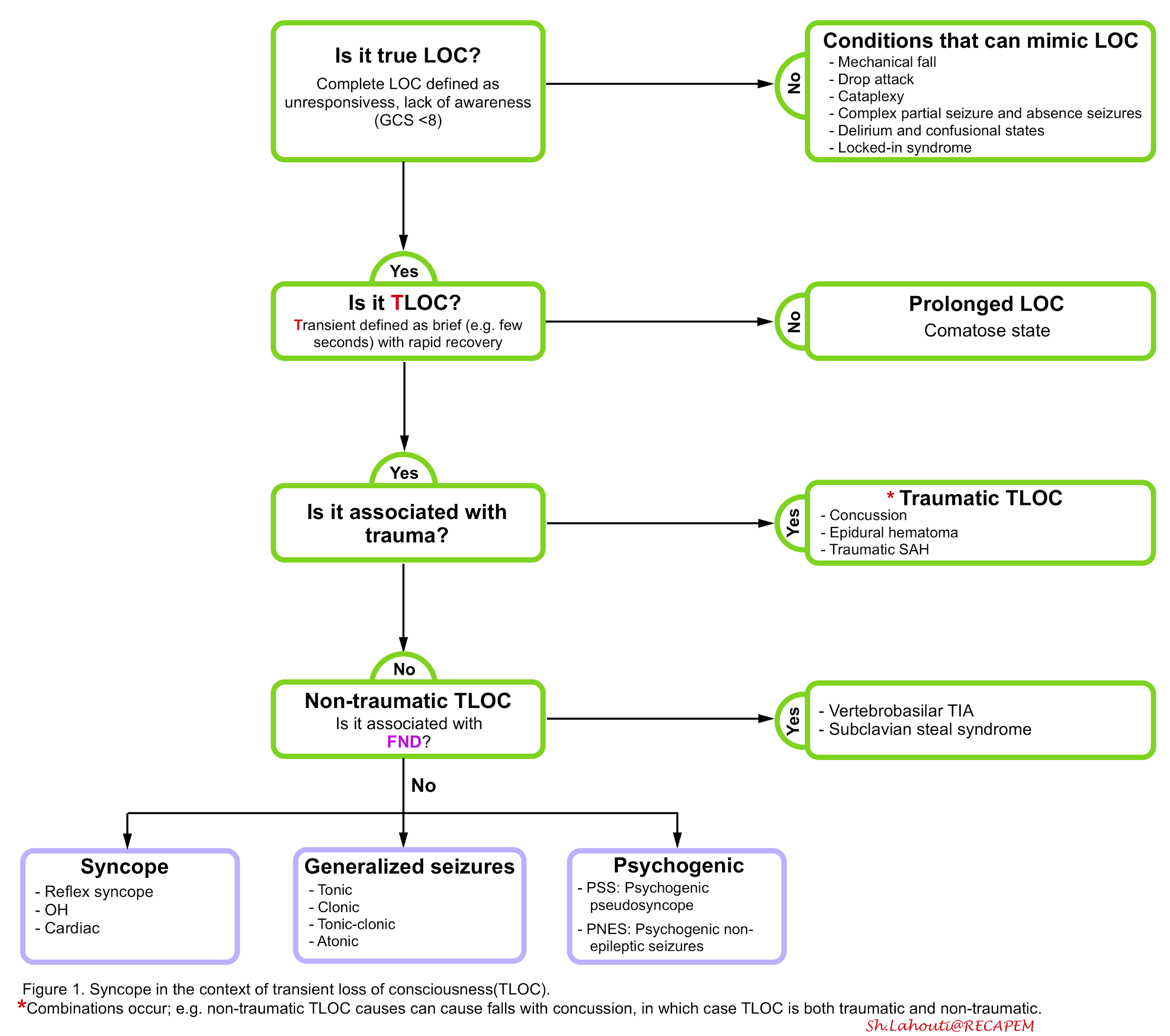
Consciousness has two domains, wakefulness (arousal) and awareness. Arousal is governed by the integrated function of different parts of the central nervous system including the reticular activating system (RAS) located within the upper and posterior part of brainstem, thalamus and the major neuronal projections to bilateral cerebral hemisphere.
- LOC results from dysfunction of either upper brain stem or bilateral cerebral hemisphere and thalamus.
- It could be transient (which is the focus of this discussion) or more prolonged (e.g. coma which will be discussed separately).
- The two main groups of TLOC are ‘TLOC due to head trauma’ and ‘non-traumatic TLOC’ (which is covered in this discussion). The non-traumatic group of TLOC is defined based on the pathophysiology as:
- Syncope: The qualifying criterion for syncope is cerebral hypoperfusion
- Epileptic seizures: Abnormal excessive brain activity
- Psychogenic TLOC: Psychological process of conversion
Syncope
- Syncope is a cardiovascular symptom.
- Regardless of the underlying causes of the syncope(figure 2), the final common pathway is interrupted blood flow for a short period of time (e.g. 8-10 seconds) to both cerebral cortices or to the brainstem ‘RAS’ resulting in transient loss of consciousness.
- The transient nature of this symptom and absence of any neurologic deficit embedded in the definition of syncope virtually makes other disease processes (e.g TIA, metabolic causes such as hypoglycemia etc.) highly unlikely to cause syncope.
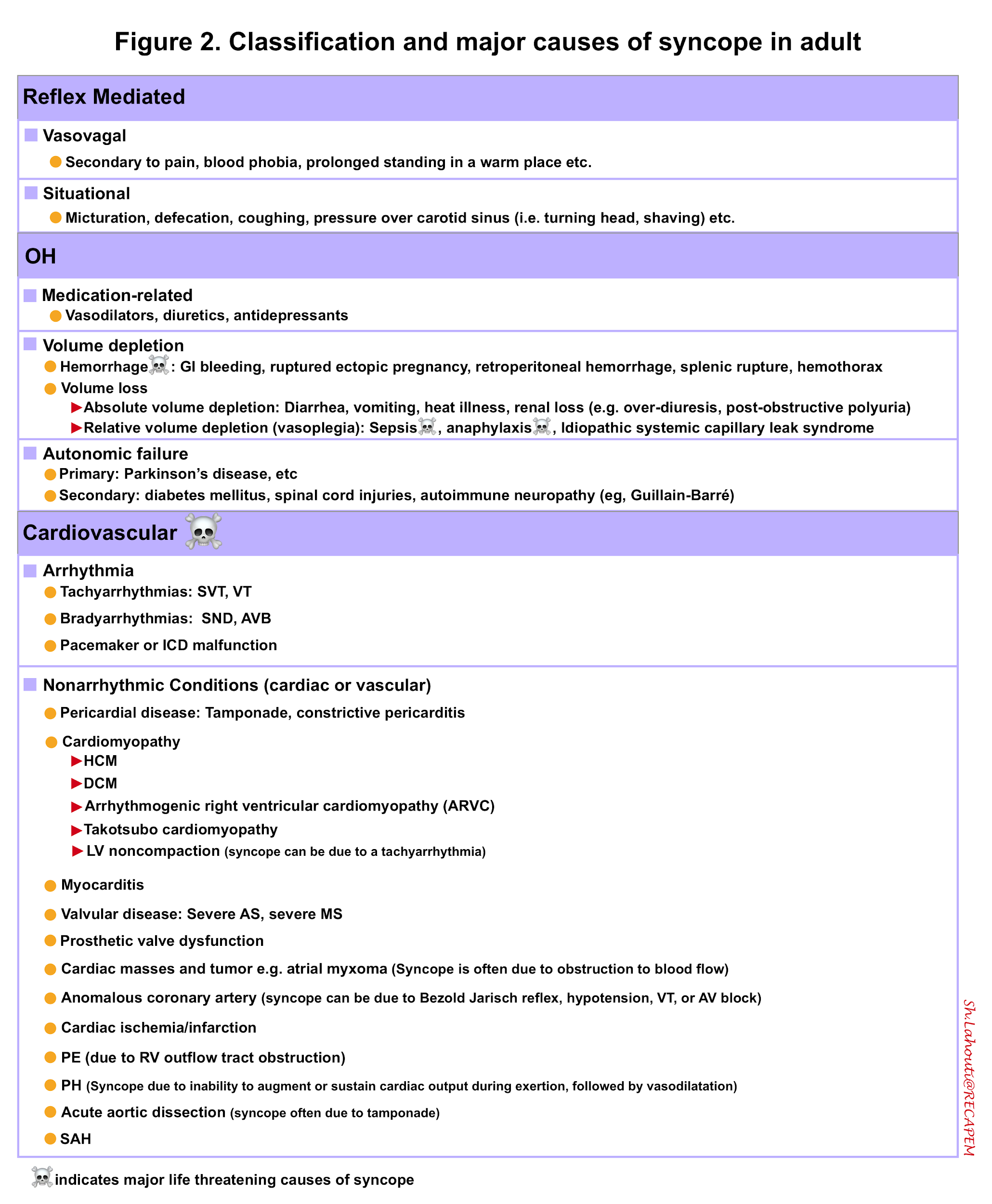
- The pathophysiologic classification of the syncope (which centers on a fall in systemic blood pressure and decrease in global cerebral blood flow) defines syncope in three classes (figure 2):
-
- Reflex mediated syncope
- Orthostatic hypotension
- Cardiac syncope
Etiology
The classified principal causes of the syncope are provided in the following figure (fig.2).
Evaluation of Syncope in ED
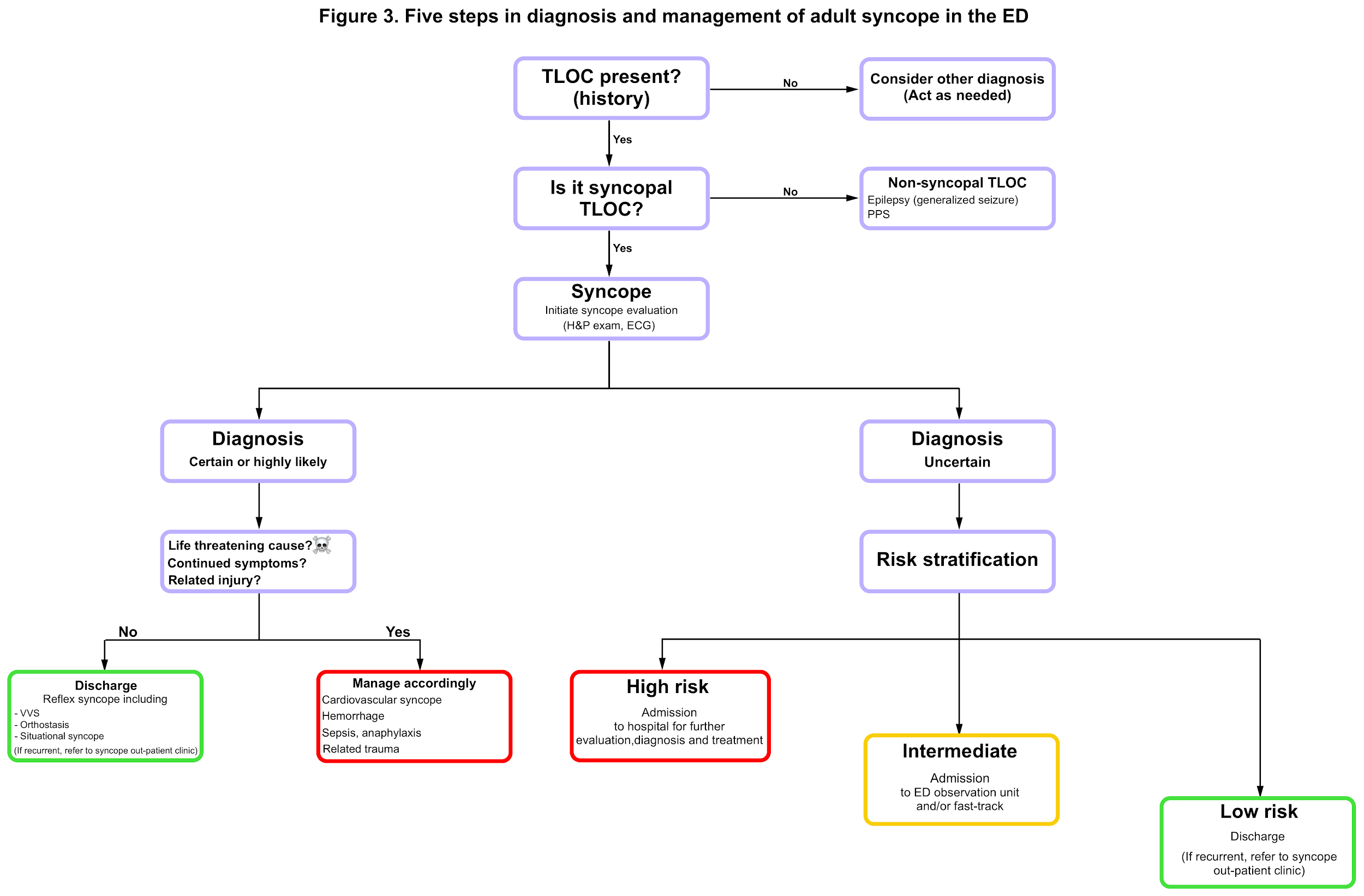
- The initial evaluation of syncope should answer the five key questions including (figure 3)4
-
- Was the event TLOC?
- In the case of TLOC, is it of syncopal or non-syncopal origin?
- In case of suspected syncope, is there a clear etiological diagnosis or a life threatening cause?
- If it’s true syncope and the cause is not clear, Is there evidence to suggest a high risk of cardiovascular events or death? (Risk stratification)
- Should the patient be admitted to hospital?
1# Was the event TLOC?
- By definition the LOC associated with syncope is transient (for a short period of time usually seconds) and self-limited (i.e. patients spontaneously recover without medical intervention). The following conditions do not meet this definition and are not considered syncope
-
- Coma: since the LOC in comatose patients are prolonged (e.g. > 1h)
- Cardiac arrest: since there’s no spontaneous recovery.
- Metabolic disorders such as hypoglycemia, hypoxia; since unless you do not correct the underlying metabolic condition, the patient will not gain consciousness spontaneously.
2# In the case of TLOC, is it of syncopal or non-syncopal origin?
- The pathophysiology of syncope is brief (6-8s) of global cerebral hypoperfusion. This brevity explains why neurologic deficit or prolonged confusion (i.e. more than 10 seconds after the attack) is not seen among patients with syncope.
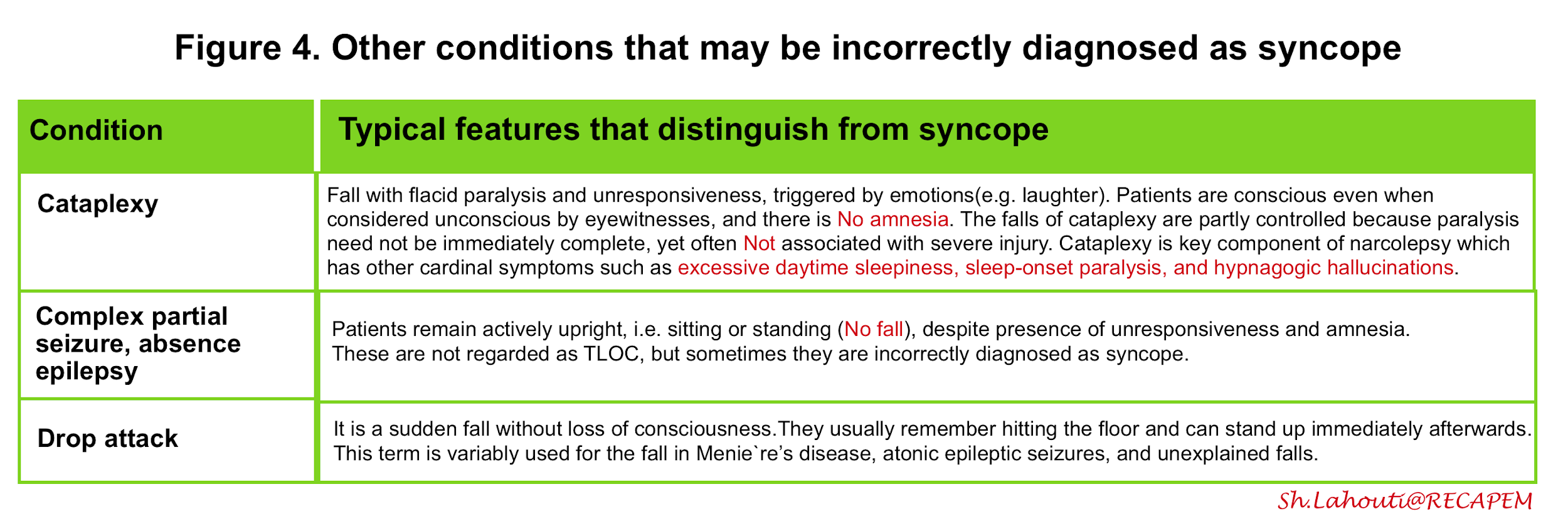
- The following conditions do not obviously meet this definition are not considered in syncope classification:
- Vertebrobasilar TIA: There’s almost always some degrees of neurologic deficit accompanied by TIA.
- Subclavian steal syndrome: Patients often have focal neurological deficit
- The only true differential diagnosis for syncope is generalized seizure and psychogenic causes.
- Generalized seizure: Sometimes it is challenging to distinguish syncope from seizure. The most helpful clues in favor of seizure are prolonged postictal confusion and tonic-clonic phase as well as prior history of epilepsy. Features such as incontinence, myoclonus during the event can happen in both syncope and seizure.
- Psychogenic syncope: The duration and the frequency of the event is helpful to differentiate it from true syncope. In psychogenic syncope, the duration of apparent LOC is longer, usually lasting many minutes to hours. There is usually no recognisable trigger, and no sweating, pallor, or nausea beforehand. The frequency of the event can be high up to several times a day. The gold standard for PPS is documenting an attack with a home video recorder or with a tilt testing during which BP, HR, and EEG are normal.
- Other conditions which may be mistaken for syncope are listed in the following table (figure 4).
3# In case of suspected syncope, is there a clear etiological diagnosis or a life threatening cause?
- The next step after identifying syncope (as a symptom) is to determine the cause, especially those life threatening conditions associated with syncope (figure 2☠️).
- By using a detailed history, focused physical examination including vitals and ECG; physicians can identify a clear etiology for syncope in approximately 60% of cases7.
- If suspected of serious causes, performing POCUS is extremely helpful.
History and physical exam
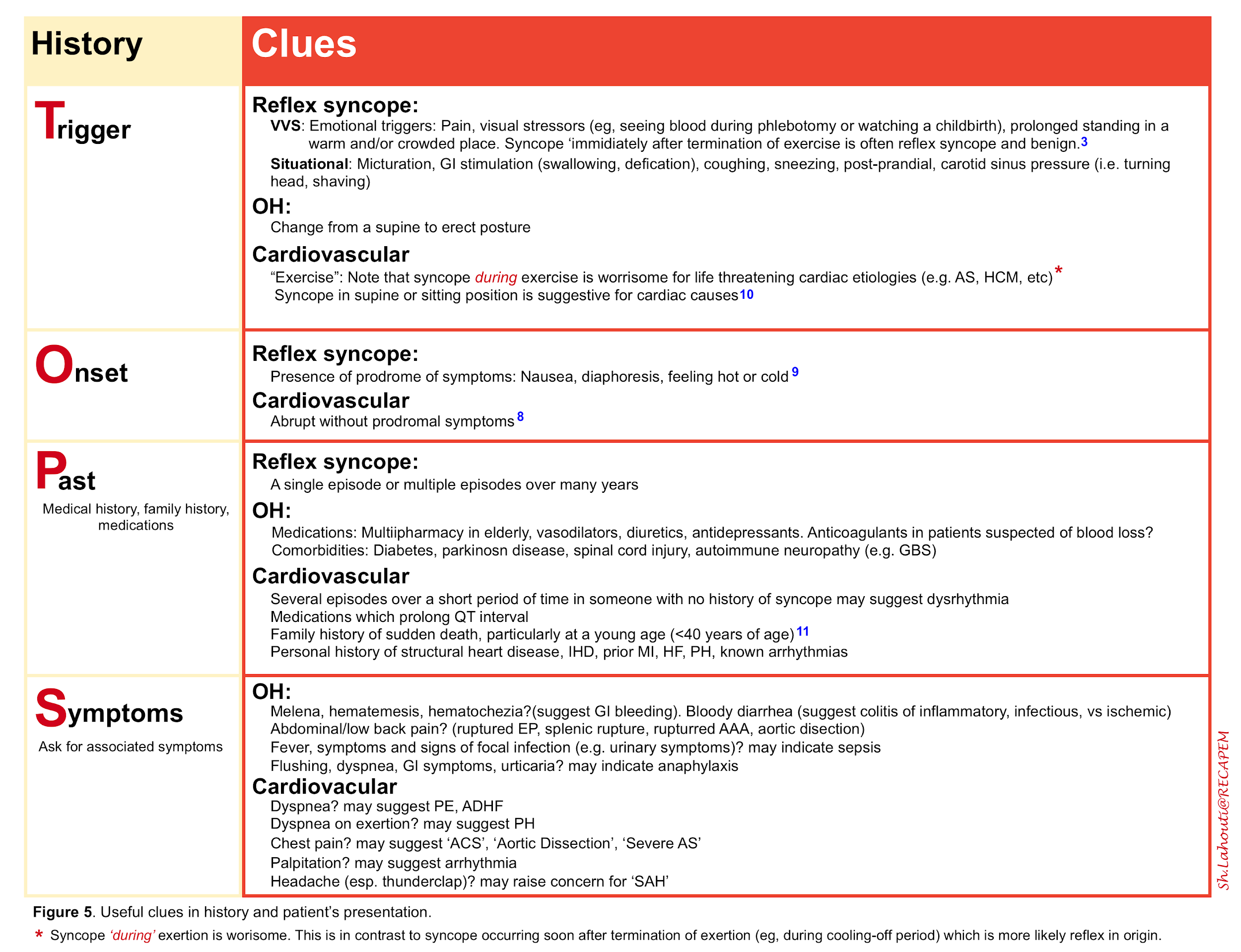
A thorough history is crucial to determine the underlying cause of syncope and possible related injury. Pay specific attention to the possible triggers, onset of the event (with or without prodrome), prior episodes, family history of unexplained sudden death at young age, patient’s list of medication, comorbidities (e.g. history of IHD, HF, etc) and possible associated symptoms (figure 5).
Physical examination
- Look for syncope-related injuries (especially elderly frail patients may develop serious head injuries following a syncopal event).
- Pay attention to persistent abnormal vital signs and perform a focused neurological exam. Other system examinations are guided by clinical presentation.
- Orthostatic vitals measurement is useless in ED for identifying underlying high risk conditions12.
- Even if performed, abnormal findings do not rule out other causes of syncope. Keep in mind that syncope from ‘OH’ is a diagnosis of exclusion in the ED, reserved for low-risk patients who have symptoms consistent with the diagnosis.
ECG
It is a simple and available test that is important for risk stratification despite that it’s rarely diagnostic 3.
- An abnormal ECG in a patient with syncope is concerning.
- By enlarge, ECGs that are changed from a previous ECG, a non-sinus rhythm, and any conduction abnormality, especially a left bundle branch block (LBBB), are most concerning13.
Bedside Ultrasound
If you are highly suspicious of underlying life threatening causes of syncope, performing POCUS can provide crucial information and facilitate appropriate management.
- Conditions where POCUS could be significantly helpful may include (but not limited to):
- Syncope and chest pain or dyspnea
- Syncope and abdominal/low back pain
- Syncope during exertion
- Syncope with persistently abnormal vital signs
- Syncope in patients with history of cardiorespiratory disorders
- Bedside echo is being more performed today by emergency physicians and can show pericardial effusion, valvular abnormalities such as aortic or mitral stenosis, wall motion abnormalities, and supportive evidence for PE (e.g. elevated pulmonary pressure, abnormal TAPSE) and aortic dissection3 .
Other investigations
Any additional laboratory or imaging tests should be directed by the results of the medical history and physical exam, and no test other than an ECG should be considered routinely.
- Cardiac monitoring
- Indicated when there is suspicion for arrhythmias.
- Keep in mind that Patients with cardiac syncope due to a lethal arrhythmia are often asymptomatic on ED presentation.
- Blood tests
- Extensive blood tests are futile.Targeted blood test is reasonable on the basis of clinical assessment in the evaluation of selected patients3 :
- Blood count: when hemorrhage is suspected
- Coagulation studies: Indicated in appropriate clinical context (e.g. anticoagulant use, history of coagulation disorder)
- Troponin: Only when cardiac ischemia is highly suspected
- D-dimer: when PE is suspected in selected patients
- Extensive blood tests are futile.Targeted blood test is reasonable on the basis of clinical assessment in the evaluation of selected patients3 :
- Imaging: only indicated and guided by clinical findings for example:
- Head CT: Only in patients where history and exam suggest ‘SAH’ or syncope related head trauma
- Other imaging modalities: may be considered in appropriate clinical context for patients with highly suspected serious conditions such as PE (CTPA), aortic dissection (CT angiography), intra abdominal hemorrhage (abdominopelvic CT with intravenous contrast).
Diagnosis
Even if there is no independent gold/reference standard to diagnose syncope, there is strong consensus that the initial evaluation may lead to certain or highly likely diagnosis when the diagnostic criteria listed below are met4 .
Reflex syncope
- Diagnosis is highly probable when any following finding were met:
- VVS: if syncope is precipitated by pain, fear, or standing, and is associated with typical progressive prodrome (pallor, sweating, and/or nausea)
- Situational reflex syncope is highly probable if syncope occurs during or immediately after specific triggers such as micturition, GI stimulation, coughing, sneezing, carotid sinus pressure
- Diagnosis is suggested when following findings are present:
- Long history of recurrent syncope, in particular occurring before the age of 40 years
- After unpleasant sight, sound, smell, or pain
- Prolonged standing
- During meal
- Being in crowded and/or hot places
- Autonomic activation before syncope: pallor, sweating, and/ or nausea/vomiting
- With head rotation or pressure on carotid sinus (as in tumours, shaving, tight collars)
- Absence of heart disease
Syncope due to OH
- Diagnosis is highly probable when syncope occurs while standing and there is concomitant significant OH.
- Diagnosis is suggested when following findings are present:
- While or after standing
- Prolonged standing
- Standing after exertion
- Postprandial hypotension
- Temporal relationship with start or changes of dosage of vasodepressive drugs or diuretics leading to hypotension
- Presence of autonomic neuropathy or parkinsonism
- Absence of heart disease
Cardiac syncope
- Arrhythmic syncope
- It is highly probable when the ECG shows:
- Persistent sinus bradycardia < 40 beats per minute or sinus pauses >3 seconds in awake state
- Mobitz II second degree AV block
- Third degree (complete) AV block
- Alternating left and right BBB
- VT or rapid paroxysmal SVT
- Non-sustained episodes of PMVT and long or short QT interval
- Pacemaker or ICD malfunction with cardiac pauses
- Arrhythmic syncope is suggested when following findings are present:
- During exertion or when supine
- Sudden onset palpitation immediately followed by syncope (absence of prodrome)
- Family history of unexplained sudden death at young age
- Presence of structural heart disease or CAD
- ECG findings suggesting arrhythmic syncope:
- Bifascicular block (defined as either left or right BBB combined with left anterior or left posterior fascicular block)
- Other intraventricular conduction abnormalities (QRS duration ≧0.12 s)
- Mobitz I second-degree AV block
- First degree AV block with markedly prolonged PR interval
- Asymptomatic mild inappropriate sinus bradycardia (40–50 b.p.m.) or slow AF (40–50 b.p.m.) in the absence of negatively chronotropic medications
- Non-sustained VT
- Pre-excited QRS complexes suggestive for WPW syndrome
- Long or short QT intervals
- Early repolarization
- ST-segment elevation with type 1 morphology in leads V1-V3 (Brugada pattern)
- Negative T waves in right precordial leads, epsilon waves suggestive of ARVC
- LVH suggesting HCM
- It is highly probable when the ECG shows:
- Cardiac ischemia-related syncope is confirmed when patients with syncope present evidence of acute myocardial ischaemia with or without myocardial infarction.
- Syncope due to structural cardiopulmonary disorders is highly probable when syncope presents in patients with prolapsing atrial myxoma, left atrial ball thrombus, severe AS, PE, or acute aortic dissection.
Risk stratification
Despite a thorough medical history and physical exam, a clear etiology will not be determined in many ED patients with syncope. In these cases, risk stratification can help to guide disposition 3.
Multiple studies have been performed to identify variables associated with ED patients at risk of both short-term and 1-year morbidity and mortality (e.g. San Francisco Syncope Rule, Canadian Syncope Risk Score etc).
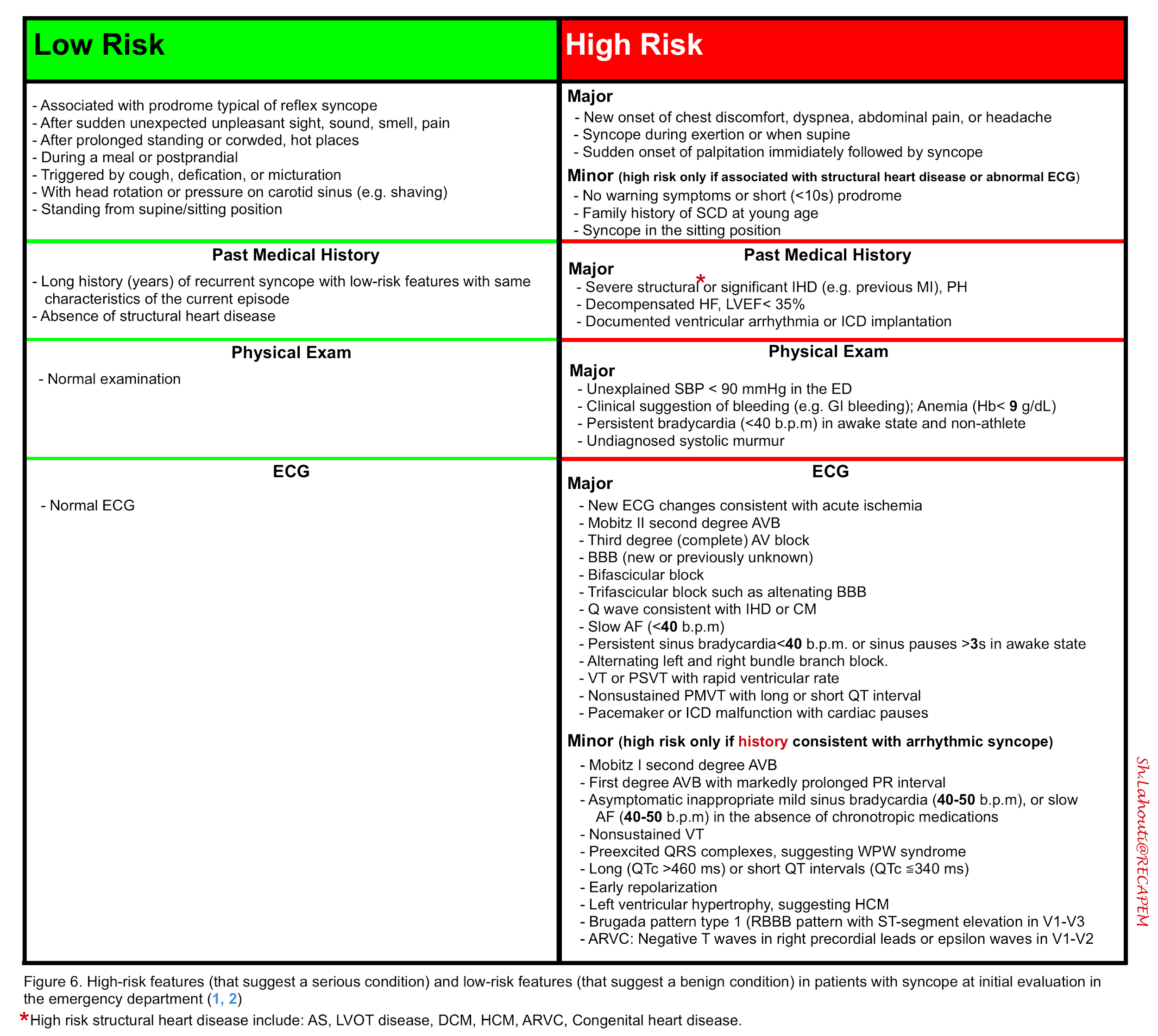
The recommendation from the 2018 European Society of Cardiology guidelines lists the following clinical variables associated with low and high risk for serious conditions (serious conditions include cardiovascular causes of syncope such as arrhythmia or other life threatening causes such as bleeding) 4.
- Among the high risk group, there are two subcategories:
- Major risk factors
- In the presence of these risk factors, it is highly probable that syncope is related to arrhythmia or other life threatening causes.
- Minor risk factors
- In the presence of these risk factors, patients are classified to intermediate risk for short-term morbidity and mortality.
- However if the history and clinical presentation suggest cardiac syncope, presence of these risk factors then move the patient’s classification up to a high risk group.
- In the presence of these risk factors, patients are classified to intermediate risk for short-term morbidity and mortality.
- Major risk factors
Management and disposition
- If the diagnosis is clear, then patients can be dispositioned accordingly (figure 3), that is to say:
- Patients with clear diagnosis of reflex syncope can be discharged home safely from ED.
- Patients with clear diagnosis of cardiac syncope or other life threatening conditions such as active GI bleeding should be admitted to the hospital for further evaluation and treatment.
- If etiologic diagnosis is not clear after initial evaluation, then patients are dispositioned based on risk stratification and clinical judgment:
- Patients in high-risk group are admitted to the hospital, while those in low-risk group can be discharged home. Patients in the intermediate-risk group benefit from a period of observation and monitoring in the observation unit.
Specific condition
Syncope in patients with comorbidity and frailty
The approach to the assessment and management of an older patient with syncope is similar to that of other age groups; however, there are a number of additional features pertinent to age-related comorbidity and frailty that warrant special attention 4. Let’s explore these in the following clinical scenario.
- A 75 y/o man collapsed in front of his wife after leaving the table having just completed his evening meal. As per his wife he looked vacant and lost his color, and then collapsed. There was an initial brief period of arm jerking. He was unconscious for 2-3min and then came round, but he was a bit confused and a little weaker than usual down the left side. She thinks that he’s back to normal 1h after the event.
- PMH: Right middle cerebral artery ischemic infarction two years ago with a good recovery, HTN, Alzheimer disease
- DH: ASA, Statin, Metoprolol, Diltiazem, Ramipril, Selegiline, Memantine, Donepezil
- Initial vitals are within normal range except for sinus bradycardia with HR of 40 b.p.m.
- He is alert and oriented x2. Exam is remarkable for mild Left arm/leg weakness compatible with his old records. Bedside echocardiography showed left ventricular hypertrophy with moderate aortic valve calcification and restriction in opening during systole.Despite extensive evaluation including brain MRI with DWI; no clear etiology was found.
Comorbidity influences the diagnosis of syncope and management decisions.
- Older patients frequently have abnormal findings on more than one investigation and may have more than one possible cause of syncope4.
- Conversely, coincidental findings of cardiovascular diagnoses such as ‘AS’ or ‘AF’ may not necessarily be the attributable cause of events.
- Focal neurological events can occasionally occur due to hypotension and syncope, even in patients without significant carotid artery stenosis (so called ‘hypotensive TIA’).
- Although these neurological events occur in only 6% of patients with recurrent syncope, their misdiagnosis is particularly important because they may lead to a lowering of BP with antihypertensive medications (e.g. if focal neurology is mistakenly attributed to vascular pathology rather than hypotension), and to a further increase of the risk of syncope and neurologic events14.
- The prescription of polypharmacy, cardiovascular, psychotropic and dopaminergic medications also increases the risk of syncope and falls.
- Negative dromotropic and chronotropic medications should be carefully evaluated in older patients presenting with syncope or falls.
- Despite the lack of large controlled trials, there is strong consensus that reduction or discontinuation of hypotensive drugs and psychotropic drugs clearly outweighs the undesirable effects of high BP4.
In our patient, the brief left arm and leg weakness is due to global cerebral hypoperfusion accentuating the weakness from his previous stroke. Adjustment of his medications was considered.
Going further
- Syncope (EM:RAP)
- Pediatric Syncope and Adult Syncope (Emergency medicine cases)
- Syncope (FOAMcast)
- Orthostatic vital signs don’t help (First 10EM)
References
1. Probst MA, Kanzaria HK, Gbedemah M, Richardson LD, Sun BC. National trends in resource utilization associated with ED visits for syncope. Am J Emerg Med. 2015 Aug;33(8):998-1001. doi: 10.1016/j.ajem.2015.04.030. Epub 2015 Apr 24. PMID: 25943042; PMCID: PMC4480060
2. Chen L, Chen MH, Larson MG, Evans J, Benjamin EJ, Levy D. Risk factors for syncope in a community-based sample (the Framingham Heart Study). Am J Cardiol. 2000 May 15;85(10):1189-93. doi: 10.1016/s0002-9149(00)00726-8. PMID: 10801999
3. Shen WK, Sheldon RS, Benditt DG, Cohen MI, Forman DE, Goldberger ZD, Grubb BP, Hamdan MH, Krahn AD, Link MS, Olshansky B, Raj SR, Sandhu RK, Sorajja D, Sun BC, Yancy CW. 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2017 Aug 1;136(5):e25-e59. doi: 10.1161/CIR.0000000000000498. Epub 2017 Mar 9. Erratum in: Circulation. 2017 Oct 17;136(16):e269-e270. PMID: 28280232.
4. Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martín A, Probst V, Reed MJ, Rice CP, Sutton R, Ungar A, van Dijk JG; ESC Scientific Document Group. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J. 2018 Jun 1;39(21):1883-1948. doi: 10.1093/eurheartj/ehy037. PMID: 29562304
5. Grossman SA, Babineau M, Burke L, Kancharla A, Mottley L, Nencioni A, Shapiro NI. Do outcomes of near syncope parallel syncope? Am J Emerg Med. 2012 Jan;30(1):203-6. doi: 10.1016/j.ajem.2010.11.001. Epub 2010 Dec 24. PMID: 21185670
6. Thiruganasambandamoorthy V, Stiell IG, Wells GA, Vaidyanathan A, Mukarram M, Taljaard M. Outcomes in presyncope patients: a prospective cohort study. Ann Emerg Med. 2015 Mar;65(3):268-276.e6. doi: 10.1016/j.annemergmed.2014.07.452. Epub 2014 Aug 30. PMID: 25182542
7. van Dijk N, Boer KR, Colman N, Bakker A, Stam J, van Grieken JJ, Wilde AA, Linzer M, Reitsma JB, Wieling W. High diagnostic yield and accuracy of history, physical examination, and ECG in patients with transient loss of consciousness in FAST: the Fainting Assessment study. J Cardiovasc Electrophysiol. 2008 Jan;19(1):48-55. doi: 10.1111/j.1540-8167.2007.00984.x. Epub 2007 Oct 3. PMID: 17916139
8. Calkins H, Shyr Y, Frumin H, Schork A, Morady F. The value of the clinical history in the differentiation of syncope due to ventricular tachycardia, atrioventricular block, and neurocardiogenic syncope. Am J Med. 1995 Apr;98(4):365-73. doi: 10.1016/S0002-9343(99)80315-5. PMID: 7709949
9. Soteriades ES, Evans JC, Larson MG, Chen MH, Chen L, Benjamin EJ, Levy D. Incidence and prognosis of syncope. N Engl J Med. 2002 Sep 19;347(12):878-85. doi: 10.1056/NEJMoa012407. PMID: 12239256
10. Alboni P, Brignole M, Menozzi C, Raviele A, Del Rosso A, Dinelli M, Solano A, Bottoni N. Diagnostic value of history in patients with syncope with or without heart disease. J Am Coll Cardiol. 2001 Jun 1;37(7):1921-8. doi: 10.1016/s0735-1097(01)01241-4. PMID: 11401133
11. Driscoll DJ, Jacobsen SJ, Porter CJ, Wollan PC. Syncope in children and adolescents. J Am Coll Cardiol. 1997 Apr;29(5):1039-45. doi: 10.1016/s0735-1097(97)00020-x. PMID: 9120157.
12. White JL, Hollander JE, Chang AM, Nishijima DK, Lin AL, Su E, Weiss RE, Yagapen AN, Malveau SE, Adler DH, Bastani A, Baugh CW, Caterino JM, Clark CL, Diercks DB, Nicks BA, Shah MN, Stiffler KA, Storrow AB, Wilber ST, Sun BC. Orthostatic vital signs do not predict 30 day serious outcomes in older emergency department patients with syncope: A multicenter observational study. Am J Emerg Med. 2019 Dec;37(12):2215-2223. doi: 10.1016/j.ajem.2019.03.036. Epub 2019 Mar 25. PMID: 30928476; PMCID: PMC6761041.
13. Dovgalyuk J, Holstege C, Mattu A, Brady WJ. The electrocardiogram in the patient with syncope. Am J Emerg Med. 2007 Jul;25(6):688-701. doi: 10.1016/j.ajem.2006.12.016. PMID: 17606095
14. Ryan DJ, Harbison JA, Meaney JF, Rice CP, King-Kallimanis B, Kenny RA. Syncope causes transient focal neurological symptoms. QJM. 2015 Sep;108(9):711-8. doi: 10.1093/qjmed/hcv005. Epub 2015 Jan 27. PMID: 25630908.






Add comment