1, December 2022, by Shahriar Lahouti.
CONTENTS
- Preface
- Presentation and diagnosis
- Stages of shock
- Epidemiology and causes of shock
- Evaluating for the causes of shock
- Initial stabilization
- Specific therapies
- Going further
- References
Preface
Shock is the clinical expression of circulatory failure. It is defined as a state of systemic hypoperfusion causing inadequate oxygen delivery to the tissues to meet cellular metabolic needs, resulting in cellular and tissue hypoxia. The effects of shock are initially reversible, but it rapidly becomes irreversible, resulting in multiorgan failure (MOF) and death. In this post the classification, etiologies and approach to diagnosis and initial stabilization of undifferentiated shock is reviewed.
Presentation and diagnosis
Recognition of shock requires a clinical judgment based on constellation of signs and symptoms augmented by bedside imaging and laboratory analysis.
General consideration
- Importance of early recognition of shock state
- The effects of shock are initially reversible, but can rapidly become irreversible, resulting in multiorgan failure (MOF) and death. Early detection and intervention are critical for improving a patient’s chance of survival.
- Pitfalls of diagnosis and management of shock
- Unfortunately there is no sign, symptom, or lab which is entirely sensitive or specific for shock. For example a normal blood pressure or normal mental status cannot rule out shock state. A normal lactate level does not exclude shock as well.
- The clinical presentation is not uniform.
- Presentation can be variable based on the severity, underlying cause(s), and patient’s physiologic reserve. For example, shock is typically associated with hypotension and reduced cardiac output, but it can also occur with normal (or even elevated) blood pressure and an increased cardiac output.
- 👉It is important to keep in mind that shock is not synonymous with hypotension.
- Presentation can be variable based on the severity, underlying cause(s), and patient’s physiologic reserve. For example, shock is typically associated with hypotension and reduced cardiac output, but it can also occur with normal (or even elevated) blood pressure and an increased cardiac output.
- Many patients with shock have a combination of more than one form of shock (multifactorial shock), for example a patient with obstructive shock due to pulmonary embolism who has concurrent ongoing GI bleeding.
- Most patients have an abnormal baseline (e.g. chronically reduced ejection fraction, CKD, dementia). This may also lead to a confusing multifactorial picture. For example a patient with history of advanced congestive heart failure who develop urosepsis.
- 👉Evaluating the archival data (e.g. old ECGs and echo) may help to sort out chronic pathology versus acute pathology.
- Certain forms of shock share overlapping features (e.g. late septic shock may look quite similar to advanced cardiogenic shock).
- Despite thorough evaluation, the cause of shock may remain unclear (undifferentiated shock).
- 👉Keep in mind that the most common cause of shock of unclear etiology is septic shock.
Clinical presentation
The diagnosis of shock should be highly suspected in the presence of ≥ 2 of the following features:
- Hemodynamics
- Hypotension may be absolute (e.g. SBP <90 mm Hg; MAP<65 mm Hg), relative (e.g. a drop in SBP >40 mm Hg); or profound (e.g. vasopressor-dependent).
- Tachycardia. Tachycardia is an early compensatory mechanism in patients with shock.
- It can be isolated or occur in association with hypotension.
- Shock index (HR/SBP): is a more helpful way to understand tachycardia within the context of blood pressure. Shock index >~0.8 suggests significant instability and possible shock *.
- Bradycardia: Severe bradycardia (e.g. HR< 30-40 bpm) should always raise concern for shock (even in normotensive patients).
- Blood pressure can be maintained by compensatory systemic vasoconstriction, while cardiac output and perfusion may still be poor.
- Tachypnea. It is an early compensatory mechanism in patients with shock and metabolic acidosis specifically.
- It is a useful tool to identify patients at risk of clinical deterioration, as evidenced by its incorporation into the qSOFA score.
- Oliguria: a urine output <0.5 mL/kg/h is worrisome for renal malperfusion *.
- Immediately following Foley catheter placement the urine output won’t be known. In this situation scanty and dark urine is worrisome.
- Urine output should be monitored by Foley catheter placement early in the ED course, as an accurate estimation requires at least 30 min of collection.
- During early resuscitation, urine production is considered normal for >1 mL/kg/h, mildly reduced for 0.5-1 mL/kg/h, and severely reduced for <0.5 mL/kg/h.
- Mental status changes. New onset of change in baseline sensorium can be a sign of shock state *.
- It is a continuum that begins with agitation, progresses to confusion or delirium, and ends in obtundation or coma.
- However, altered mental status is neither sensitive nor specific.
- Delirium is not a specific symptom for shock. The list of etiologies causing altered mentation is broad. In fact most new-onset delirium isn’t due to shock.
- Delirium is not a sensitive symptom for shock. Normal mental status does not rule out hypoperfusion state.
- In fact most patients with cardiogenic shock often have normal mentation despite poor perfusion of other organs.
- In contrast, patients with sepsis more often develop delirium (delirium tends to be a feature of septic shock rather than of cardiogenic shock).
- Skin perfusion status
- Cool, clammy skin is due to compensatory peripheral vasoconstriction that redirects blood centrally, to maintain vital organ perfusion (i.e. coronary, cerebral, and splanchnic flow) *.
- Caveats:
- A cool, clammy or cyanotic skin may also be due to the underlying peripheral arterial vascular disease.
- A warm, hyperemic skin does not exclude the absence of shock because such an appearance may be present in patients with early distributive shock (prior to the onset of compensatory vasoconstriction) or terminal shock (due to failure of compensatory vasoconstriction).
- Caveats:
- Mottling is less sensitive, but more specific for hypoperfusion and elevated mortality *. A cyanotic, mottled appearance is a late and worrisome feature of shock.
- Mottling suggests active endogenous vasoconstriction, implying that the patient would benefit from an increase in cardiac output (e.g. an inotrope), rather than additional exogenous vasoconstrictors.
- Urticaria, angioedema, and pruritus are suggestive of anaphylaxis; when in doubt start empiric therapy for anaphylaxis immediately.
- Cool, clammy skin is due to compensatory peripheral vasoconstriction that redirects blood centrally, to maintain vital organ perfusion (i.e. coronary, cerebral, and splanchnic flow) *.
- Elevated Lactate (e.g. >4 mM) suggests shock *, but this has a broad differential diagnosis *.
- An elevated serum lactate is an early indicator of shock * and is particularly useful in identification of occult shock (those who are normotensive or even hypertensive).
- High lactate level is worrisome. This should be interpreted in appropriate clinical context. It can represent shock or some other impending disaster until proven otherwise *.
- Normal lactate isn’t necessarily reassuring (can occur in shock).
- In practice lactate usually doesn’t reflect oxygen deficiency, but rather endogenous epinephrine in response to physiologic stress. This explains why lactate can be normal in shocked patients who have inadequate sympathetic nervous function.
- More on lactate: Understanding lactate in sepsis & Using it to our advantage(PULMCrit)
Stages of shock
Shock is a physiologic continuum; begining with an inciting event, such as a focus of infection (e.g. abscess) or an injury (e.g. gunshot wound), triggering pathophysiological changes, which can progress through several stages.
- Compensated shock (aka. occult shock, impending shock, cryptic shock)
- It is characterized by compensatory responses to diminished tissue perfusion.
- As an example, in early hypovolemic pre-shock, a compensatory tachycardia and peripheral vasoconstriction may allow an otherwise healthy adult to be asymptomatic and preserve a normal or mildly elevated blood pressure despite a 10% reduction in total effective arterial blood volume.
- Signs and symptoms: Tachycardia, a modest change in systemic blood pressure (increase or decrease), or mild to moderate hyperlactatemia, may be the only clinical signs of early shock.
- It is potentially important to recognize this early stage. As with timely and appropriate management, deterioration can be prevented and signs of impending deterioration can be reversed (e.g. normalization of heart rate and serum lactate levels).
- It is characterized by compensatory responses to diminished tissue perfusion.
- Frank (overt) shock
- The compensatory mechanisms become overwhelmed, and signs and symptoms of multiple (≧2) organs organ dysfunction appear including: symptomatic tachycardia, dyspnea, agitation, diaphoresis, metabolic acidosis, hypotension, oliguria, and cool, clammy skin.
- End-organ dysfunction
- Progressive shock leads to irreversible organ damage, multiorgan failure (MOF), and death.
- During this stage, anuria and acute renal failure develop, acidemia further depresses cardiac output, hypotension becomes severe and recalcitrant to therapy (often related to vasoplegia), and agitation evolves into obtundation and coma.
- Typically patients Impending to cardiorespiratory arrest (from any cause) present with:
- Obtundation
- Accessory use of respiratory muscle, agonal breathing, or RR < 10.
- Mottling, cyanosis, diaphoresis
- MAP < 40 mm Hg.
- HR < 30 bpm.
- VT/VF.
- Several scoring systems have been designed to predict and evaluate the outcome of critically ill patients by employing most relevant clinical parameters for prediction of mortality. Example include: APACHE II Score, SOFA Score ,qSOFA Score, and NEWS 2 Score.
- Note that these scoring systems are designed to quantify disease severity and facilitate identifying of patients who are at greater risk of death.
Epidemiology and causes of shock
It is estimated that more than 1.2 million annual ED visits are for patients in shock *. Shock is common in the critically ill population, occurring in a third of patients admitted to the ICU.
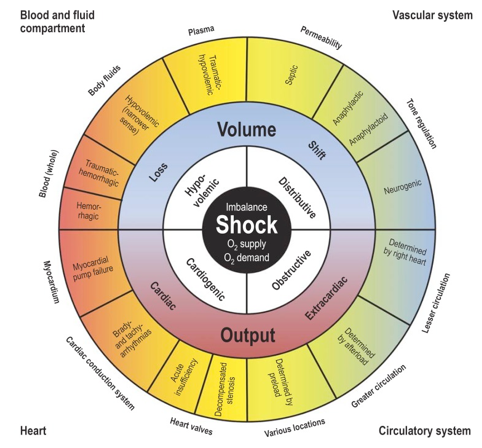
Several life-threatening processes can cause shock. Classically 4 categories of shock have been described *.
- Distributive shock (vasodilatory shock): The most common class of shock.
- Septic shock (~62%)*
- Non-septic (~4%)
- Inflammatory shock (severe systemic inflammatory response syndrome)
- Pancreatitis, post-cardiac arrest, burns, trauma, postmyocardial infarction, post coronary bypass, post cardiac arrest, amniotic fluid embolism, fat embolism.
- Anaphylaxis
- Neurogenic shock (severe CNS/spinal trauma, spinal anesthesia)
- Others:
- Adrenal crisis, thyroid storm
- Liver failure
- Toxic shock syndrome
- Transfusion reactions
- Vasoplegia: Excess vasodilatory drug, cardiopulmonary bypass
- Inflammatory shock (severe systemic inflammatory response syndrome)
- Hypovolemic (~16%)
- Hypovolemic (e.g. vomiting, diarrhea, over-diuresis, post-ATN or postobstructive polyuria, DKA).
- Hemorrhagic
- Gastrointestinal bleeding (e.g. varices, peptic ulcer)
- Retroperitoneal bleeding (e.g. ruptured aortic aneurysm)
- Aortoenteric fistula
- Ruptured ectopic pregnancy
- Spontaneous peritoneal hemorrhage from bleeding diathesis
- Postpartum bleeding
- Hemothorax
- Cardiogenic (~16%)
- Arrhythmogenic
- Tachyarrhythmia (usually >170 bpm)
- Bradyarrhythmia (usually < 30-40 bpm)
- LV failure (non-mechanical)
- Myocardial infarction (involving >40% of the left ventricle or with extensive ischemia)
- Myocarditis, postpartum cardiomyopathy
- Drug-induced: Beta blockers and calcium channel blocker overdose.
- LV failure (mechanical)
- Severe valvular insufficiency e.g. AR, MR.
- LVOTO
- RV failure
- Severe right ventricle infarction
- Massive pulmonary embolism
- Decompensated chronic pulmonary hypertension
- Arrhythmogenic
- Obstructive (~2%)
- Tension pneumothorax
- Tamponade
- Abdominal compartment syndrome
- AutoPEEP or high mean airway pressures
👉Mortality rates for patients in shock vary drastically based on the etiology, but the common causes of shock, including sepsis, trauma, and cardiac failure, have mortality rates of 20-50%.
Evaluating the cause of shock
Determination of the category and etiology of shock can guide the appropriate therapy. However, in these critically ill patients, it is imperative to evaluate/think/act simultaneously.
- Do NOT wait to gather a complete history or perform a full physical examination prior to formulating a working differential diagnosis and initiating appropriate interventions *.
- ⏳Time is Tissue: Hemodynamic stabilization must be prompted before identifying the cause of shock.
History can provide important clues as to the etiology of shock
- Current medications & changes in medication list.
- Cardiac history (cardiovascular risk factors, any prior information about cardiac structure/function such as ECG, echo).
- Risk factors for venous thromboembolism
- Adrenal disease (patients chronically on oral steroid may be assumed to be insufficient).
- Risk factors for systemic infections such as
- Immunosuppression, invasive devices (e.g. hemodialysis catheters), IV drug user and splenectomized patients.
- Previous procedures or trauma, for example:
- The aortoenteric fistula (AEF) must be kept in mind as a possible etiology of GI bleeding in any patient with known AAA or prior aortic intervention, no matter how long ago.
- AEF may present with abdominal pain, hematemesis, hematochezia.
Specific signs and symptoms
🚩Some specific signs and symptoms can potentially suggest certain causes of shock in appropriate clinical context.
- Chest pain, dyspnea (AMI, acute aortic syndrome, PE)
- Abdominal/back pain (ruptured AAA)
- Leg size discrepancy (PE)
- Fever, shaking chills, productive cough, lower urinary tract symptoms, peritoneal signs, skin rashes (sepsis)
- Hematemesis, hematochezia, melena (GI bleeding)
Labs
- Lactate
- CBC and differentiation
- Renal and liver function tests.
- Extended electrolytes
- Coagulation profile
- Troponin (in patient suspected for AMI)
- D-dimer
- A value lower than cut off (adjusted for age *) in patient with a low to intermediate pretest probability of having a pulmonary embolism, can rule out PE.
- BNP
- A BNP level < 100 pg/ml or N-terminal-proBNP < 300 pg/ml indicate that acute HF is unlikely *.
- Sepsis evaluation
- Infectious workup if sepsis is suspected (e.g. blood cultures, urinalysis and culture)
- Procalcitonin: If a decision has been made to treat empirically with antibiotics, then check a procalcitonin as well.
- Type & cross-match blood if hemorrhage suspected
- Endocrine evaluation
- Cortisol level if adrenal insufficiency is possible
- TSH if thyroid storm suspected
ECG is used to identify arrhythmias, ischemia, or changes consistent with certain toxidromes.
Imaging
- CXR (e.g. may reveal pneumonia or cardiogenic edema implying LV failure)
- CT depending on clinical scenario (e.g. CTA to evaluate for PE, CT abdomen/pelvis to exclude septic focus in abdomen, CT angio of abdomen to look for hemorrhage).
- POCUS: is important for identifying the etiology of hypoperfusion * and monitoring responses to therapy at any point during resuscitation.
- Multiple POCUS protocols (ACES, BLUE , RUSH, FALLS, etc.) have been proposed for the early and rapid evaluation of patients in shock. It has been shown that early use of POCUS in evaluation of patients in shock is helpful to identify the etiology or at least the category of shock *.
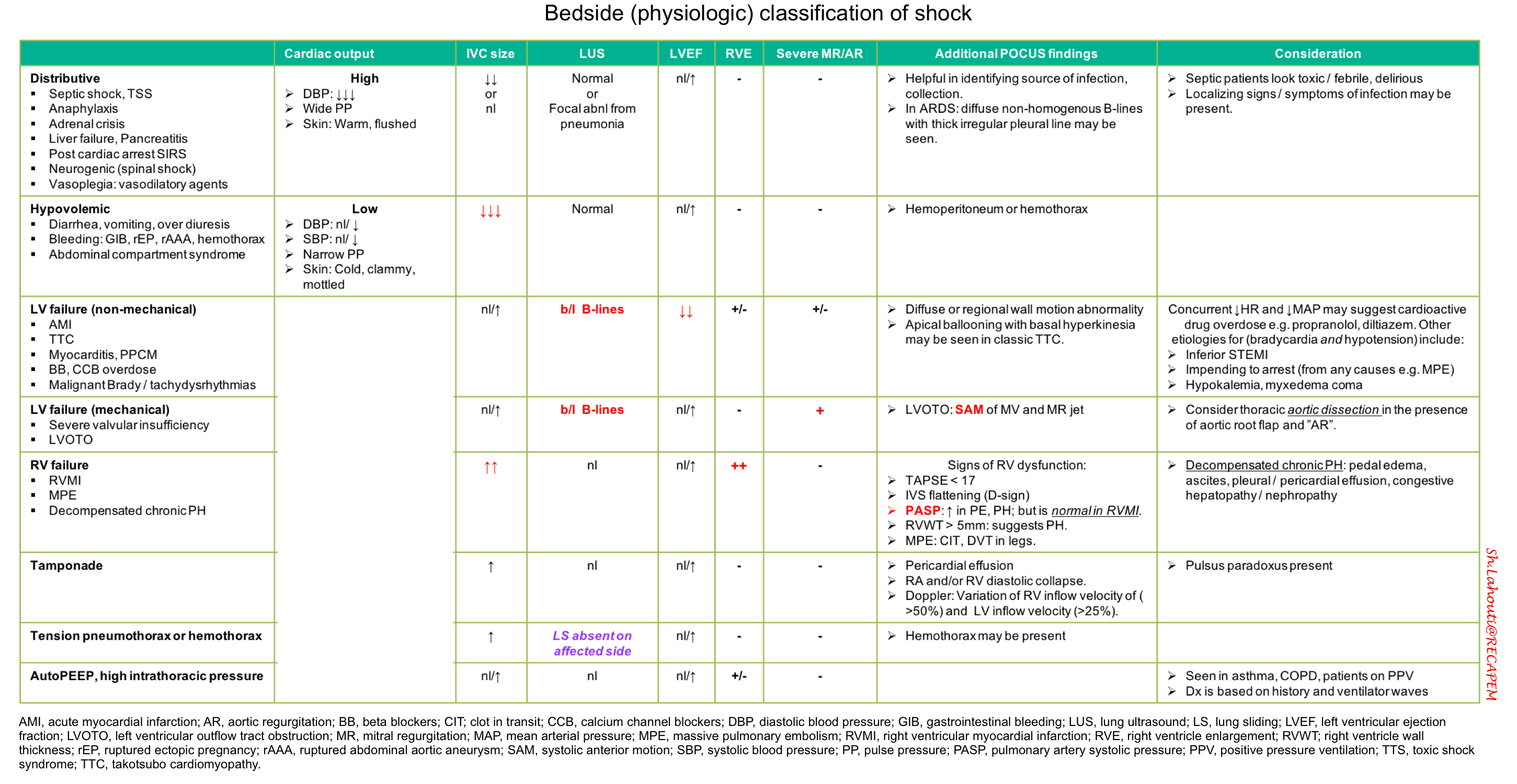
Bedside physiologic classification of shock
Findings on ultrasonography and physical examination may be integrated for bedside physiologic classification of shock (table below).
- This works best in previously-healthy patients with a single mechanism of shock.
- Patients with multiple chronic problems or multifactorial shock may defy classification .
- Septic shock is the most common type of shock in critically ill patients.
- If initial evaluation fails to reveal any obvious cause of shock, septic shock is likely and it is imperative to treat empirically for sepsis.
Initial stabilization
Approach all patients in a systematic fashion using an airway, breathing, circulation methodology.
Airway
- If intubation is indicated, correct hypotension with push-dose pressors before proceeding for intubation.
- ⚠️Avoid intubation (and positive pressure ventilation) if possible in patients with suspected obstructive shock (pulmonary embolism, tension pneumothorax, cardiac tamponade).
Breathing
-
Administer supplemental oxygen targeting saturation (SpO2) of 90%-94%.
-
Consider non-invasive positive pressure ventilation (CPAP or BiPAP) for patients with cardiogenic pulmonary edema.
Circulation
- Basic principles
- In the presence of multiple hemodynamics derangement, consider treatment strategies in following sequence order:
- Correct the “HR” first, if dysrhythmia is suspected as the primary cause of hemodynamic instability. Dysrhythmia is likely the primary cause of hemodynamic instability, if
- HR < 30-40 bpm
- AF with rapid ventricular response > 150 bpm
- Non-sinus tachycardia > 170 bpm
- Second: Correct volume status (if appropriate) before correcting resistance problem.
- Third: Correct resistance problems (e.g. by vasopressors) to rapidly improve tissue perfusion.
- Fourth: Consider inotropic support (if indicated).
- Correct the “HR” first, if dysrhythmia is suspected as the primary cause of hemodynamic instability. Dysrhythmia is likely the primary cause of hemodynamic instability, if
- In the presence of multiple hemodynamics derangement, consider treatment strategies in following sequence order:
- Access
- Establish ≥2 large-bore peripheral IVs, a central venous line, or intraosseous access to allow for high-volume fluid resuscitation and vasopressor administration.
- Fluid
- Fluid is often provided in boluses fashion (e.g. 500 ml) with attention to patient response.
- Consider using a balanced crystalloid solution (e.g. lactated Ringer’s solution) over normal saline.
- The total amount of fluid administered should generally be limited to <1-2 liters in the absence of a history suggesting substantial total-body volume depletion (e.g. severe diarrhea).
- Even patients with end-stage renal disease and severe congestive heart failure may need adequate volume resuscitation with frequent reassessments, especially if the shock etiology is hypovolemic or distributive.
- Hold IV fluid, if signs of pulmonary edema are present on exam or bedside ultrasound.
- Boluses of fluid is often recommended except for few clinical conditions:
- Bilateral B-line in lung ultrasound. This patients may have LV failure and pulmonary edema.
- A dilated IVC without respiratory collapsibility. These patients have an elevated filling pressures and are unlikely to benefit from fluid.
- Fluid administration can be diagnostic and therapeutic in confusing situations where hypovolemia is suspected:
- If fluid resuscitation alone resolves the shock, this supports a diagnosis of hypovolemia.
- If fluid resuscitation fails, this suggests an alternative diagnosis. This is especially true if fluid resuscitation results in adequate filling pressures (e.g. full IVC) without resolving the shock.
- Fluid is often provided in boluses fashion (e.g. 500 ml) with attention to patient response.
- Vasopressor
- Vasopressor administration should be started immediately if the blood pressure is inadequate (e.g. MAP<65 mm) and in peri-cardiac (impending) arrest *.
- Pressors may be administered via peripheral vein (except for vasopressin).
-
Norepinephrine infusion (0.01-3 μg/kg/min) is the first-line vasopressor for undifferentiated shock, along with suspected septic, cardiogenic, and neurogenic shock.
-
Epinephrine infusion (0.01-0.1 μg/kg/min) is an appropriate alternative to norepinephrine for undifferentiated shock, especially in bradycardic peri-arrest.
-
In cases of suspected anaphylaxis, intramuscular epinephrine (1:1000) 0.1-0.5 mg (max 1 mg) followed by epinephrine infusion is the first-line treatment for ongoing shock.
-
-
Vasopressin infusion (0.01-0.1 units/min) can be added for continued hypotension.
-
Typically given in low doses (0-0.06 U/min), either as primary or secondary agent.
-
- Inotropic support
- Dobutamine infusion (2-20 μg/kg/min) (max 40 μg/kg/min) can be added if low cardiac output is suspected in patients with signs of ongoing hypoperfusion despite adequate intravascular volume and an appropriate dose of vasopressors.
Antibiotic
- If sepsis is possible, cultures should be performed and empiric antibiotics should be started without delay.
- Have a low threshold to give an empiric dose of antibiotic for undifferentiated hypotension in ED.
- In patients with possible sepsis, you don’t necessarily need to go extremely broad with the antibiotics. A single broad-spectrum agent may be reasonable (e.g., piperacillin-tazobactam).
Steroid
- Indicated for patients whom you suspect have adrenal crisis, for example:
- Patients with known adrenal insufficiency
- Patients taking chronic steroids who recently missed doses.
- Septic shock with persistent instability after appropriate fluid and vasopressor therapy.
Specific therapies
Every attempt should be made to identify and treat the underlying cause of shock. Once the diagnosis is known, specific therapies should be refined, and the response to therapy monitored. Additional targeted therapies for specific shock etiologies may include:
- Suspected cardiogenic shock due to ACS: Consult cardiology for potential early invasive therapy with cardiac catheterization followed by percutaneous coronary intervention or coronary artery bypass grafting. More on this 👉 here.
- Suspected cardiogenic shock resulting from a dysrhythmia: Follow the ACLS pathways.
- Bradyarrhythmia here and tachydysrhythmias here.
- AF is the most common arrhythmia in critically ill patient. See more on 👉 management of AF.
- Valvular emergencies: 👉 Acute severe AR,👉 acute severe MR and 👉 dynamic LVOTO.
- RV failure:
- 👉Principles of RV failure management.
- 👉MPE. For suspected MPE leading to obstructive shock, consider thrombolysis.
- 👉Decompensated PH.
- 👉Management of tamponade.
- 👉Management of acute aortic syndromes
- Tension pneumothorax:
- Emergent needle decompression (using 14-16 gauge IV catheter) followed by tube thoracostomy is indicated.
- If endotracheal intubation is indicated (for other reasons, e.g. bleeding into airway in head trauma), it is preferred to do decompression of tension pneumothorax before the intubation; unless the patient is in cardiac arrest.
Top image: Synoptic view of the four types of shock (inner, white field) with the organ systems primarily associated with them (outer corners), sites and mechanisms of manifestation (outside the circle), and pathogenetic and pathophysiologic features (outer and middle sectors of the circle). To maintain clarity, mixed types of shock are not depicted. PMID: 30573009
Going further
- The Hypotensive ED Patient: A Sequential Systematic Approach (emDocs)
- Approach to shock (IBCC)
- An approach to undifferentiated hypotension (First 10 in EM)
- Algorithm for the Evaluation of Hypotension
- Undifferentiated shock (WikEM)
References
1.Tseng J, Nugent K. Utility of the shock index in patients with sepsis. Am J Med Sci. 2015 Jun;349(6):531-5. doi: 10.1097/MAJ.0000000000000444.
2. van Diepen S, Katz JN, Albert NM, Henry TD, Jacobs AK, Kapur NK, Kilic A, Menon V, Ohman EM, Sweitzer NK, Thiele H, Washam JB, Cohen MG; American Heart Association Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; and Mission: Lifeline. Contemporary Management of Cardiogenic Shock: A Scientific Statement From the American Heart Association. Circulation. 2017 Oct 17;136(16):e232-e268. doi: 10.1161/CIR.0000000000000525. Epub 2017 Sep 18.
3. Galbois A, Bigé N, Pichereau C, Boëlle PY, Baudel JL, Bourcier S, Maury E, Guidet B, Ait-Oufella H. Exploration of skin perfusion in cirrhotic patients with septic shock. J Hepatol. 2015 Mar;62(3):549-55. doi: 10.1016/j.jhep.2014.10.012. Epub 2014 Oct 19.
4. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med. 2017 Mar;45(3):486-552. doi: 10.1097/CCM.0000000000002255.
5. Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014 Dec 11;371(24):2309-19. doi: 10.1056/NEJMra1309483.
6. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10. doi: 10.1001/jama.2016.0287.
7. Mellhammar L, Linder A, Tverring J, Christensson B, Boyd JH, Sendi P, Åkesson P, Kahn F. NEWS2 is Superior to qSOFA in Detecting Sepsis with Organ Dysfunction in the Emergency Department. J Clin Med. 2019 Jul 29;8(8):1128. doi: 10.3390/jcm8081128.
8. Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008 Aug 6;(7):1-38.
9. Standl T, Annecke T, Cascorbi I, Heller AR, Sabashnikov A, Teske W. The Nomenclature, Definition and Distinction of Types of Shock. Dtsch Arztebl Int. 2018 Nov 9;115(45):757-768. doi: 10.3238/arztebl.2018.0757.
10. Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013 Oct 31;369(18):1726-34. doi: 10.1056/NEJMra1208943.
11. Righini M, Van Es J, Den Exter PL, Roy PM, Verschuren F, Ghuysen A, Rutschmann OT, Sanchez O, Jaffrelot M, Trinh-Duc A, Le Gall C, Moustafa F, Principe A, Van Houten AA, Ten Wolde M, Douma RA, Hazelaar G, Erkens PM, Van Kralingen KW, Grootenboers MJ, Durian MF, Cheung YW, Meyer G, Bounameaux H, Huisman MV, Kamphuisen PW, Le Gal G. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism: the ADJUST-PE study. JAMA. 2014 Mar 19;311(11):1117-24. doi: 10.1001/jama.2014.2135. Erratum in: JAMA. 2014 Apr 23-30;311(16):1694.
12. Martindale JL, Wakai A, Collins SP, Levy PD, Diercks D, Hiestand BC, Fermann GJ, deSouza I, Sinert R. Diagnosing Acute Heart Failure in the Emergency Department: A Systematic Review and Meta-analysis. Acad Emerg Med. 2016 Mar;23(3):223-42. doi: 10.1111/acem.12878. Epub 2016 Feb 13.
13. Perera P, Mailhot T, Riley D, Mandavia D. The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically lll. Emerg Med Clin North Am. 2010 Feb;28(1):29-56, vii. doi: 10.1016/j.emc.2009.09.010
14. Atkinson PR, Milne J, Diegelmann L, Lamprecht H, Stander M, Lussier D, Pham C, Henneberry R, Fraser JM, Howlett MK, Mekwan J, Ramrattan B, Middleton J, van Hoving DJ, Peach M, Taylor L, Dahn T, Hurley S, MacSween K, Richardson LR, Stoica G, Hunter S, Olszynski PA, Lewis DA. Does Point-of-Care Ultrasonography Improve Clinical Outcomes in Emergency Department Patients With Undifferentiated Hypotension? An International Randomized Controlled Trial From the SHoC-ED Investigators. Ann Emerg Med. 2018 Oct;72(4):478-489. doi: 10.1016/j.annemergmed.2018.04.002. Epub 2018 Jun 2.
15. Gidwani H, Gómez H. The crashing patient: hemodynamic collapse. Curr Opin Crit Care. 2017 Dec;23(6):533-540. doi: 10.1097/MCC.0000000000000451.




Add comment